What are uterine anomalies or uterine abnormalities?
Uterine anomalies, also known as uterine abnormalities, refer to variations in the structure of the uterus. Uterus is the female organ of reproduction and it is essential for childbearing. It is the organ where the embryo implants after fertilization and where the baby grows. It is normally a pear-shaped organ with a cavity. Some women may have different size, shape, or structure of the uterus and those are called uterine anomalies. These anomalies can include septate uterus (a wall or partition within the cavity of the uterus), bicornuate uterus (heart-shaped), unicornuate uterus (one-sided), didelphic uterus (double uterus), arcuate uterus (mild indention at the top) and a mix of these can also be seen.
These variations are generally present from birth and sometimes may impact a woman’s childbearing capacity.
What are the types of uterine abnormalities?
There are several types of uterine abnormalities, each characterized by specific changes in the structure of the uterus. The common types are:
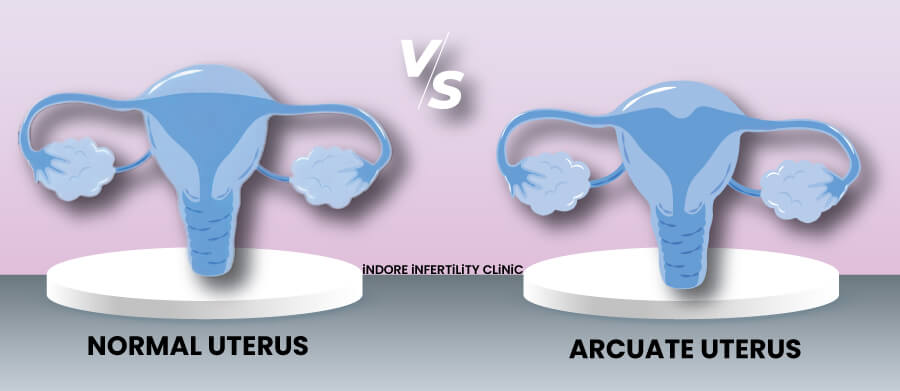
- Arcuate Uterus: A mild indention at the top of the uterus. Generally considered a minor anomaly with minimal impact on pregnancy, but it can cause recurrent miscarriage.
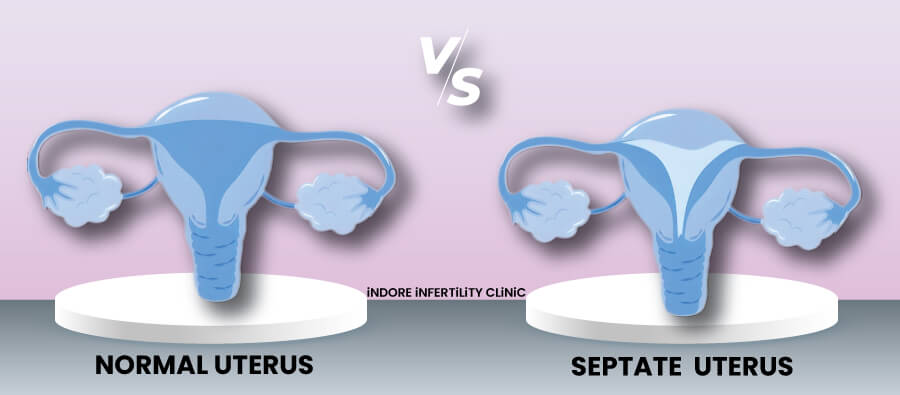
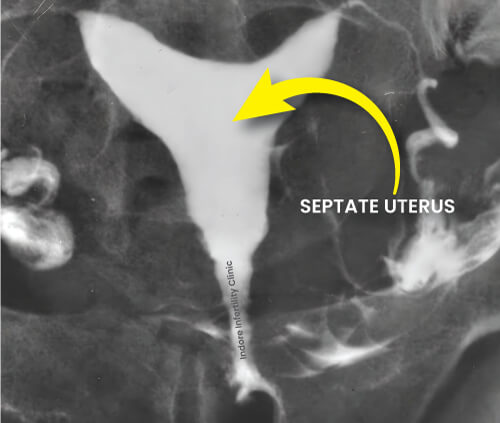
- Septate Uterus: A septate uterus has a wall or partition (septum) within the uterine cavity, dividing it partially or completely. It may increase the risk of recurrent miscarriages or preterm birth (birth before 37 weeks of pregnancy).
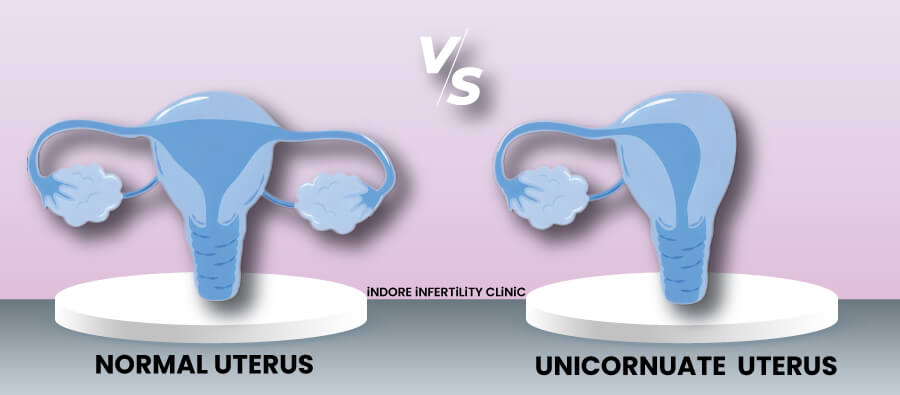
- Unicornuate Uterus: The uterus is shaped like a single horn, with one side not fully developed. It has a higher risk of complications such as preterm birth and breech presentation (the baby is bottom first positioned in the uterus).
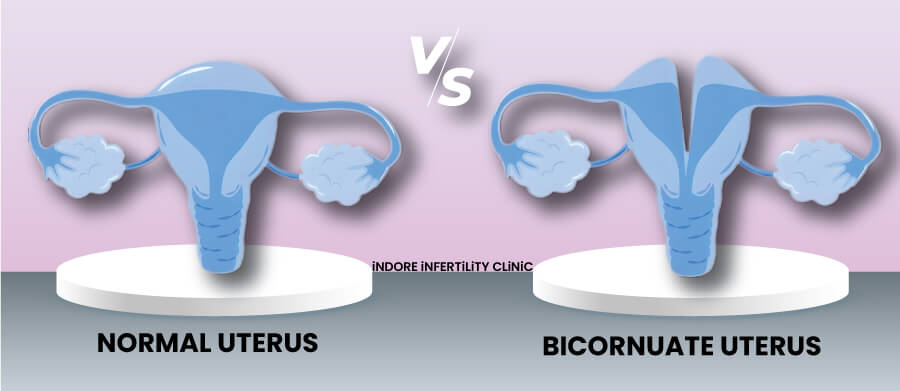
- Bicornuate Uterus: The uterus has a heart-shaped appearance due to a dip in the middle. It may increase the risk of recurrent miscarriage and preterm birth.
- Didelphic Uterus: The uterus is double, forming two separate structures. It may increase the risk of preterm birth and pregnancy-related complications.
What are the symptoms of uterine abnormality?
Women with uterine abnormalities often do not experience significant symptoms, and many of them may not be aware of it until they face fertility problems or experience complications during pregnancy. Some potential symptoms of uterine anomalies are:
- Menstrual Problems: having irregular, heavy or painful periods. They can also have increased pelvic discomfort around menses.
- Recurrent Miscarriages: having multiple miscarriages without an apparent cause.
- Difficulty in getting pregnant
- Preterm Birth or Pregnancy Complications: risk of preterm birth and other complications like abnormal position of the baby in uterus.
How common is uterine abnormality?
Uterine abnormalities are relatively uncommon, but their prevalence can vary depending on the specific type of anomaly. In general population congenital uterine anomalies are present in 0.1-3.8% women, but they are seen in 6.7% in women with infertility.
-
SEPTATE UTERUS - 35%
Accounts for approximately 35% of all uterine anomalies.
-
BICORNUATE UTERUS - 25%
Represents about 25% of uterine anomalies.
-
UNICORNUATE UTERUS - 20%
Makes up around 20% of uterine anomalies.
-
DIDELPHIC UTERUS - 8%
Seen in about 8% of uterine anomalies.
-
ARCUATE UTERUS - 6% TO 11%
Considered a milder form and is found in around 6-11% of uterine anomalies.
How is uterine abnormality diagnosed?
A uterine anomaly can be diagnosed by following means:
- Medical History and Physical Examination: Your doctor will ask about your menstrual history, reproductive history, and any symptoms you may be experiencing.
A pelvic examination might be needed along with this.
- Ultrasound: Transvaginal ultrasound is often used for evaluating the uterus. It provides detailed images and allows your doctor to visualize the uterus.
- 3D ultrasound: A three-dimensional image of the uterus can be created and is very useful in assessment of uterine anomalies.
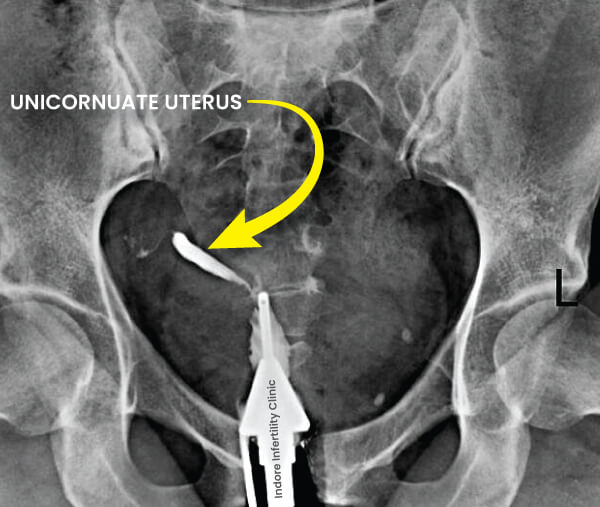
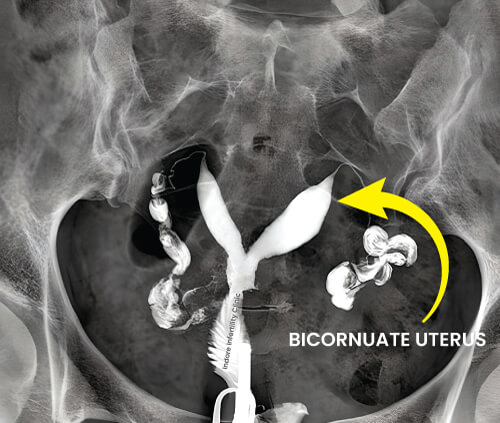
- Hysterosalpingography (HSG): HSG is a special X-ray procedure in which a contrast dye is injected into the uterus from the cervix. This dye helps outline the uterine cavity and fallopian tubes, making it easier to identify any abnormalities.
- Hysteroscopy: Hysteroscopy is a minimally invasive procedure where a thin tube (hysteroscope) is inserted through the cervix into the uterus. This allows direct visualization of the uterine cavity and any abnormalities.
- Magnetic Resonance Imaging (MRI): In some cases, MRI may be used to provide more detailed imaging of the uterus and surrounding structures, providing additional information.
- Laparoscopy: Laparoscopy is a surgical procedure that involves the insertion of a thin tube with a camera through a small incision in the abdomen. It may be used to visualize the external structure of the uterus and surrounding organs. Sometimes it can be done together with a hysteroscopy to get the inside and the outside view of the uterus and the tubes.
The choice of diagnostic method depends on various factors, including the specific symptoms, the suspected type of uterine abnormality, and the woman’s medical history and plans for pregnancy.
What are the various treatments for uterine abnormalities?
The treatment for uterine abnormalities depends on the type and severity of the anomaly, as well as the woman’s plan for pregnancy. Some common treatments approaches for different uterine abnormalities are:
- Observation and Monitoring: In cases where the uterine anomaly is mild and not causing significant issues, your gynaecologist or infertility doctor may choose a “wait and watch” approach.
- Hysteroscopic Surgery: For certain anomalies such as a septate uterus, hysteroscopic surgery may be recommended. This involves removing the septum or correcting the abnormality using specialized instruments inserted through the cervix.
- Laparoscopic Surgery: Laparoscopic surgery may be considered for certain uterine abnormalities mostly those involving the external surface of the uterus. Tube like thin instruments are introduced in the abdomen through small incisions and a camera is used to visualize and guide the whole process.
- Myomectomy: If uterine fibroids (lumps/knots in the uterus) are contributing to the abnormality, a myomectomy (removal of fibroids) may be performed. This can help restore the normal shape of the uterus and its cavity.
What is unicornuate uterus?
A unicornuate uterus is a type of congenital uterine anomaly characterized by a uterus that is shaped like a single horn or half of a uterus. This condition results from the incomplete development of one side of the Müllerian ducts (structures that give rise to the female reproductive organs) during fetal development.
Features of a unicornuate uterus:
- The uterus has a characteristic banana or hook
- One side of the uterus is either absent or minimally developed.
- The cervix and the fallopian tube on the affected side may also be underdeveloped.
- Impact on Pregnancy: Women with a unicornuate uterus may have a higher risk of pregnancy complications, including preterm birth and breech presentation (bottom first).
- The smaller size of the uterus may limit the space available for fetal growth leading to restricted growth of the baby.
- Diagnosis is typically made through imaging studies such as ultrasound or magnetic resonance imaging (MRI).
What is bicornuate uterus?
A bicornuate uterus is a congenital uterine anomaly characterized by a uterus that has a heart-shaped appearance. This condition occurs when the Müllerian ducts, which give rise to the female reproductive organs during fetal development, partially fuse but do not completely unite. The result is a uterus with a central dip or cleft at the top, creating the characteristic heart shape.
Features of a bicornuate uterus:
- The uterus has a heart or butterfly shape.
- There is a deep indentation at the top of the uterus, dividing it into two distinct compartments.
- The degree of indentation can vary, and the size of the uterus may be normal or slightly larger.
- Impact on Pregnancy: While a bicornuate uterus is generally considered a milder uterine anomaly, it may be associated with a slightly increased risk of recurrent miscarriage and preterm birth.
- The impact on fertility and pregnancy outcomes can vary among individuals.
- Diagnosis is typically made through ultrasound or magnetic resonance imaging (MRI).
What is the difference between unicornuate and bi-cornuate uterus?
Both unicornuate and bicornuate uteruses are congenital (present since birth) uterine anomalies, but they differ in their structural characteristics:
Unicornuate Uterus: A unicornuate uterus is shaped like a single horn or half of a uterus. It forms when only one side of the uterus develops fully, and the other side is either absent or minimally developed.
- Appearance: The uterus has a characteristic banana or hook shape.
- Impact on Pregnancy: Women with a unicornuate uterus may have a higher risk of pregnancy complications, including preterm birth and breech presentation, as the uterus is smaller and may not provide much space for baby’s growth.
- Sometimes there is a rudimentary horn present, and an ectopic pregnancy can implant in it.
Bicornuate Uterus: A bicornuate uterus has a heart-shaped appearance due to a dip or cleft in the middle. It results from incomplete fusion of the Müllerian ducts (structures which form the uterus) during fetal development.
- Appearance: The uterus has a heart or butterfly shape, with a deep indentation at the top.
- Impact on Pregnancy: While women with a bicornuate uterus may have a slightly increased risk of recurrent miscarriage and preterm birth, the impact on pregnancy is generally less pronounced than in cases of unicornuate uterus.
What are the risks of getting pregnant with unicornuate or bicornuate uterus?
Following are common complications in pregnancy with a unicornuate or bicornuate uterus:
- Recurrent Pregnancy Loss: Due to the abnormal shape of the uterine cavity, pregnancy sometimes doesn’t continue normally, resulting in a recurrent loss of pregnancy. This is common with unicornuate, bicornuate and septate uterus.
- Reduced Space for Baby’s Growth: The limited space in the uterus may affect the baby’s growth and development.
- Increased Risk of Preterm Birth: Due to the smaller size of the uterus in unicornuate uterus or smaller cavity in case of bicornuate uterus, there is an increased risk of preterm birth.
- Breech Presentation: Babies in a unicornuate and bicornuate uterus are more likely to be in a breech position (buttocks first).
Increased Risk of Caesarean Section: The abnormal uterine shape may increase the likelihood of needing a caesarean section delivery (C-section).
What is septate uterus? Is it very common?
A septate uterus is a type of congenital uterine anomaly characterized by a partition or wall (septum) that divides the uterine cavity. This septum may extend partially or completely from the top to the bottom of the uterus. A septate uterus forms during fetal development when the Müllerian ducts, which give rise to the female reproductive organs, do not fuse properly.
Features of a septate uterus:
- The septum may be thick or thin.
- It can either partially or completely divide the uterine cavity into two separate compartments.
- Impact on Pregnancy: Women with a septate uterus may have a higher risk of pregnancy complications, including recurrent miscarriages, preterm birth, and breech presentation (bottom first). The septum can interfere with the implantation of the embryo or baby’s growth due to reduced space.
- Diagnosis is typically made through imaging studies such as regular ultrasound or 3D sonography, hysterosalpingography (HSG), or hysteroscopy.
- Treatment: Hysteroscopic surgery is often recommended to remove the septum. This procedure involves inserting a thin, lighted tube (hysteroscope) through the cervix to visualize and remove the septum.
- Prevalence: A septate uterus is one of the more common uterine anomalies. It is estimated to occur in approximately 1-2% of women in the general population.
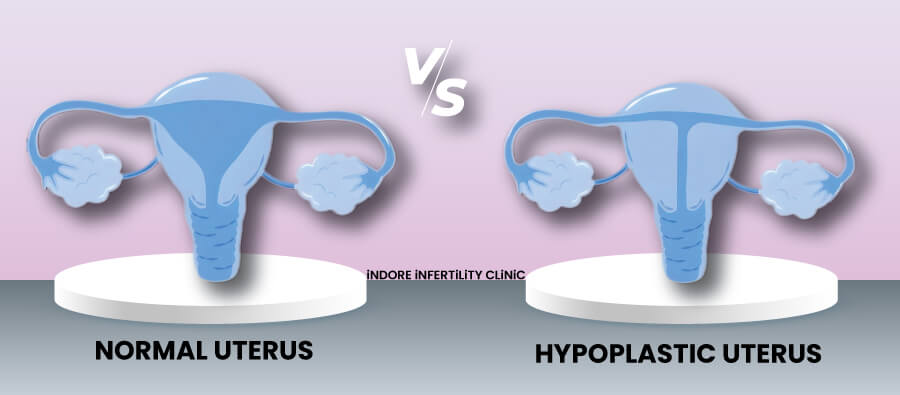
What is hypoplastic uterus?
A hypoplastic uterus refers to a uterus that is underdeveloped or smaller than usual. This congenital condition occurs during fetal development when the Müllerian ducts, which give rise to the female reproductive organs, do not develop properly and as a result, the uterus may be smaller in size than the normal.
Features of a hypoplastic uterus:
- The uterus may be smaller in length and width compared to the average uterus.
- The cervix and other reproductive structures may also be affected to varying degrees.
- Impact on Pregnancy: The impact on fertility and pregnancy can vary depending on the degree of hypoplasia.
- Women with a hypoplastic uterus may have difficulty in conceiving or maintaining a pregnancy.
- Diagnosis is typically made through imaging studies such as ultrasound or magnetic resonance imaging (MRI).
- Treatment options depend on the severity of the hypoplasia.
What is MRKH syndrome?
Mayer-Rokitansky-Küster-Hauser (MRKH) syndrome, also known as Müllerian agenesis or congenital absence of the uterus and vagina, is a rare congenital condition that affects the development of the female reproductive system. It occurs in 1 in 4500 women. It is characterized by the absence or sometimes underdevelopment of the uterus and the upper part of the vagina. Women with MRKH syndrome typically have normal external genitalia and normal secondary sexual characteristics, such as breast development and mostly have normal ovaries as well.
Features of MRKH syndrome:
- The uterus is generally absent or sometimes significantly underdeveloped.
- The upper part of the vagina may be absent or shorter than usual.
- External genitalia, including the labia and clitoris, are typically normal.
- Development of secondary sexual characteristics, such as breast development and pubic hair, is normal.
- It can be associated with some abnormalities in kidneys, ureters and spine as well in some cases.
- Women with MRKH syndrome are unable to conceive and carry a pregnancy due to the absence of the uterus.
- Ovarian function is typically normal and they can consider alternative methods for attaining motherhood such as surrogacy or adoption.
- Diagnosis is usually made during adolescence or early adulthood when a woman does not have menstruation or has difficulty with sexual intercourse.
Treatment aims at restoring normal sexual function and family planning. A vaginal cavity can be developed by use of vaginal dilators (mechanical method) and in resistant or sever cases a new vagina can be created surgically, involving a plastic surgeon. For family planning they can consider surrogacy or adoption.
Can I have a baby if I am diagnosed with MRKH?
Mayer-Rokitansky-Küster-Hauser (MRKH) syndrome is a congenital condition characterized by the absence or underdevelopment of the uterus and upper part of the vagina. While women with MRKH syndrome cannot carry a pregnancy themselves, following options are usually offered to them:
- Surrogacy: It allows the woman and her husband to become biological parents. Women with MRKH syndrome can use their own eggs (if she has functioning ovaries), fertilized with the partner’s sperm through IVF. The fertilized embryo is then implanted in a surrogate’s uterus to carry the baby for the rest of the term.
- Adoption: It is a viable option for individuals or couples who are unable to conceive or carry a pregnancy and are not considering surrogacy.
- Uterine Transplant (Experimental): Uterine transplant is an experimental procedure that involves transplanting a uterus from a living or deceased donor to a woman with MRKH syndrome. This option is still in the early stages of development, with limited availability and success rates.
Can I get pregnant with congenital uterine abnormalities?
The ability to get pregnant with congenital uterine abnormalities depends on the type and severity of the anomaly. Some women with uterine abnormalities may conceive naturally, while others may have increased risk of certain complications like miscarriages or preterm births. Here’s a general overview for different types of congenital uterine abnormalities and their impact on pregnancy:
- Unicornuate Uterus: Women with a unicornuate uterus may experience difficulty in getting pregnant due to the smaller size of the uterus. However, with careful monitoring and appropriate management, successful pregnancies are possible. They are at higher risk of preterm births.
- Bicornuate Uterus: In many cases, women with a bicornuate uterus can conceive naturally. The impact on fertility is often milder compared to certain other uterine anomalies. Laparoscopic surgery might be advised to correct the anomaly.
- Septate Uterus: Women with a septate uterus have an increased risk of recurrent miscarriages. Surgical correction of the septum through hysteroscopy can improve outcomes in these cases.
- Arcuate Uterus: An arcuate uterus is generally considered a milder anomaly, and women with this condition may have a good chance of conceiving naturally without significant impact on fertility. Hysteroscopic correction may improve pregnancy chance.
- Didelphic Uterus: Fertility may vary among women with a didelphic uterus. In some cases, conception is possible, but close monitoring during pregnancy is essential due to a higher risk of complications. Mostly it has good prognosis.
- Hypoplastic Uterus: Women with a hypoplastic uterus may have problems in conceiving naturally, and assisted reproductive technologies (ART) such as in vitro fertilization (IVF) or surrogacy may be considered.
If a woman with a congenital uterine abnormality is planning to conceive, it is advisable to consult with an infertility specialist. They can conduct a thorough evaluation, provide personalized guidance, and discuss appropriate management options based on the situation.
What are the chances of naturally conceiving with uterine abnormalities?
The chances of naturally conceiving with uterine abnormalities can vary widely depending on the type and severity of the anomaly. It is important to understand that the ovaries are generally not affected in uterine anomalies, the problem lies with the uterus, and thus either miscarriage or preterm birth is the commonest problem, rather than difficulty getting pregnant.
Here are some general considerations for different types of uterine abnormalities:
- Unicornuate Uterus: Women with a unicornuate uterus may have difficulty conceiving or maintaining pregnancy due to the smaller size of the uterus. However, many can still conceive naturally with careful monitoring and appropriate management.
- Bicornuate Uterus: Women with a bicornuate uterus often have a better chance of natural conception compared to certain other uterine anomalies. However, there may be a slightly increased risk of recurrent pregnancy loss and preterm birth.
- Septate Uterus: The impact on fertility can vary. They can conceive but mostly have problem of recurrent miscarriage, for which surgical correction might be needed.
- Didelphic Uterus: Fertility may vary among women with a didelphic uterus. Many women have normal reproductive life and are unaware of this condition, while a significant number might face difficulty getting pregnant.
- Arcuate Uterus: In many cases, women with an arcuate uterus can conceive naturally without significant impact on fertility. Surgical intervention may not always be necessary.
- Hypoplastic Uterus: Women with a hypoplastic uterus have difficulty in natural conception, and assisted reproductive technologies (ART) such as in vitro fertilization (IVF) and surrogacy may be needed.
Can congenital uterine abnormalities be treated by surgery?
Yes, many congenital uterine abnormalities can be treated surgically.
Here are some common congenital uterine abnormalities along with their surgical treatments:
- Septate Uterus: Hysteroscopic metroplasty is a minimally invasive procedure where a hysteroscope (a thin, lighted tube) is inserted through the cervix to visualize and remove the septum dividing the uterus.
- Bicornuate Uterus: Metroplasty or septoplasty can be performed to correct the indentation at the top of the uterus. The surgery may be performed through hysteroscopy or laparoscopy or open method (laparotomy).
- Unicornuate Uterus: Surgical correction may involve reconstructing the unicornuate uterus or removing the non-communicating horn to create a more normal uterine shape. The surgery may be performed through open method (laparotomy) or laparoscopy.
- Didelphic Uterus: Many of these women don’t require surgery and some are not even aware of having this condition, because of normal pregnancy and childbearing. But those who face fertility and pregnancy problems can consider surgery depending on the extent of abnormality and other associated conditions.
- Arcuate Uterus: Surgical intervention may not always be necessary for an arcuate uterus, as it is considered a milder anomaly. Hysteroscopic correction of the uterine shape is a surgery advised in such cases.
What is Adenomyosis?
Adenomyosis is a condition that occurs when the tissue that normally lines the cavity of the uterus (endometrium) begins to grow into the muscular walls of the uterus (myometrium). This results in an enlarged and thickened uterus. Adenomyosis is a benign condition, but it can cause pain and other symptoms, particularly during menstruation.
Features of adenomyosis:
- Enlarged and tender uterus: The presence of extra tissue within the uterine walls can lead to an enlargement of the uterus. The uterus may also become tender.
- Adenomyosis often occurs in women in their 30s and 40s and may cease to progress after menopause.
Symptoms of Adenomyosis:
- Often more severe than usual menstrual cramps. Pain can also start few days before menses and can last longer than the menses.
- Women with adenomyosis may experience chronic pelvic pain, discomfort, or a feeling of fullness in their pelvis.
- Heavy or prolonged menstrual bleeding, sometimes sever enough to cause anaemia or severely impact a woman’s life.
Diagnosis: Adenomyosis is often diagnosed based on symptoms and clinical examination. Imaging studies such as ultrasound or magnetic resonance imaging (MRI) may be used to confirm the diagnosis.
Treatment: depends on the severity of the symptoms and the woman’s plans for pregnancy:
- Pain management: Over-the-counter pain relievers or prescription medications may be used to manage pain.
- Hormonal therapies: Combined hormonal pills, hormonal IUDs (e.g.- Mirena), or other hormonal medications may help control symptoms of pain and excessive bleeding.
- Infertility specialist consultation: In cases where the woman is not able to get pregnant, a specialist consultation with an infertility doctor is needed. Many times, IVF may be advised as a last resort.
- Surgery: In severe cases not responding to medicines or other conservative treatments and for women who have completed their family, a hysterectomy (removal of the uterus) may be considered as a definitive treatment.
Can I get pregnant with adenomyosis?
Adenomyosis is a condition in which endometrial tissue, which normally lines the uterus, infiltrates the muscular walls of the uterus. While adenomyosis is associated with certain fertility problems, many affected women can still conceive and have successful pregnancies.
Some important points to remember about adenomyosis are:
Effect on Fertility: Adenomyosis can impact the fertility of women, but it can be variable for different women. Some women with adenomyosis can conceive naturally, while others may experience complications.
Symptoms and Severity: Women with milder form of disease may experience fewer symptoms and those with severely affected uterus may have more problems and possibly have fertility problems.
Treatment Options: The management of adenomyosis and fertility problems often involves a combination of approaches. These may include pain management, hormonal therapies to regulate the menstrual cycle, and, in some cases, surgery might be needed to remove adenomyotic tissue.
Assisted Reproductive Technologies (ART): For fertility problems arising due to adenomyosis, assisted reproductive technologies (ART), such as in vitro fertilization (IVF), may be considered.
What is endometriosis?
Endometriosis is a condition in which tissue similar to the inner lining of the uterus, called the endometrium, grows outside the uterus. This tissue can be found on the ovaries, fallopian tubes, the outer surface of the uterus, the intestines, and other pelvic structures. Endometriosis is a chronic and often painful condition that can severely impact a woman’s reproductive and overall health.
Features of endometriosis:
- Endometriosis involves the presence of endometrium-like tissue in locations outside the inner lining of the uterus.
- Inflammation and scarring: The presence of endometriosis can lead to inflammation, the formation of adhesions (scar tissue), and the development of cysts in the ovaries known as chocolate cysts of the ovaries or endometriomas.
- Painful menstruation: Women with endometriosis often experience intense menstrual cramps and chronic pelvic pain.
- Painful intercourse: Sexual intercourse may be painful for women with endometriosis.
- Infertility: Endometriosis is one of the well-known causes of infertility in women.
Symptoms of Endometriosis:
- Pelvic pain: This can range from mild discomfort to severe pain, especially during menstruation. Painful intercourse or pelvic examination can also be a feature.
- Painful bowel movements or urination: Endometriosis can affect the intestines or bladder, leading to pain during bowel movements or urination.
- Heavy menstrual bleeding: Some women with endometriosis experience heavy or prolonged menstrual bleeding.
- Fatigue and discomfort: Endometriosis can cause chronic fatigue and general discomfort.
Diagnosis: Ultrasound can be advised as a preliminary imaging test, as it can show ovarian cysts (chocolate cysts). Confirmed diagnosis is typically made through laparoscopic surgery, which allows direct visualization of the pelvic structures and the identification of endometriotic lesions. Usually, any corrective surgery is also performed in the same sitting.
Treatment options aim to manage symptoms and may include:
- Pain medication: Over-the-counter or prescription pain relievers.
- Hormonal therapies: Combined hormonal pills, hormonal IUDs (e.g.- Mirena), or other hormonal medications to regulate the menstrual cycle and reduce symptoms.
- Surgery: Laparoscopic surgery to remove endometriotic lesions, adhesions, or cysts.
- Infertility specialist consultation: In cases where there is difficulty in getting pregnant consultation with infertility doctor is recommended.
- In severe cases or when fertility is not a concern or when a woman has completed her family, a more extensive surgery such as hysterectomy (removal of uterus) with removal of ovaries may be considered.
Endometriosis and its impact on women can vary and be extremely debilitating for many women. It is a chronic condition that may require long-term management
Can I get pregnant with endometriosis?
Yes, women with endometriosis can get pregnant, but the condition is notoriously known for its association with infertility. The severity of endometriosis and its impact on fertility can vary widely among women.
Here are some important points to know:
- Fertility Problems: Endometriosis can contribute to infertility in women. The presence of endometrial tissue outside the uterus can lead to inflammation, scarring, and the formation of adhesions, potentially affecting the function of the ovaries, fallopian tubes, and uterus. They also have higher pregnancy failures.
- Individual Variations: The impact of endometriosis on fertility varies from person to person. Some women with mild endometriosis may conceive naturally, while others may not. The extent of disease does not correlate well with the symptoms and impact on fertility.
- Treatment Options: For women with endometriosis who are trying to conceive, various treatment options may be considered. These may include hormonal therapies to regulate the menstrual cycle, pain management, or surgery to remove endometrial lesions and adhesions. Fertility treatments such as in vitro fertilization (IVF) may also be recommended in some cases.
- Timing and Age: Age can be a significant factor in fertility. Women with endometriosis are advised to seek medical advice early if they have concerns about fertility, as age-related factors can increase the impact of endometriosis on their fertility.
- Assisted Reproductive Technologies (ART): Endometriosis is frequently seen in women with fertility problems, and it affects fertility by various modes. IVF can help bypass all those potential barriers and give good results. If you have endometriosis and are planning to conceive, it’s essential to consult an infertility specialist early on.
For which uterine abnormality should I consider surrogacy?
Surrogacy is usually advised in cases where the woman herself cannot carry the pregnancy, due to either absent or severely defective uterus.
Here are some uterine abnormalities for which surrogacy might be considered:
- Congenital Absence of the Uterus (Uterine Agenesis): In conditions where the uterus is completely absent (as in Mayer-Rokitansky-Küster-Hauser syndrome), surrogacy is often considered as the woman cannot carry a pregnancy herself.
- Severe Uterine Anomalies with Limited Functionality: cases like hypoplastic uterus, unicornuate uterus.
Apart from uterine anomalies, following conditions might also require surrogacy:
Hysterectomy or Uterine Removal: If a woman has undergone a hysterectomy, that is having her uterus removed due to any reason.
- Medical Conditions Impacting Uterine Function: Certain medical conditions or treatments (such as cancer treatment involving uterine radiation) can compromise uterine function.
- Problems with the endometrium (uterine lining): In certain conditions the uterus is normal externally, but the uterine lining or endometrium is not proper or not functioning normally. This includes cases like – intra-uterine adhesions, atrophied endometrium or after procedures like endometrial ablation (a treatment done for heavy uterine bleeding, involving permanent damage to endometrium).
The decision to pursue surrogacy is highly personal and involves careful consideration of one’s emotional, ethical, legal, and financial aspects. Before opting for surrogacy, it’s advisable to consult with infertility specialists, and legal professionals experienced in surrogacy arrangements.




