
How Good Is My Embryo ?
Inquisitiveness, is what makes us human. We all want to “KNOW”. Here is a blog that addresses the topic of embryo grading in as much detail as possible from a patient’s perspective. While you read on, please do remember, that medicine is not mathematics where 2 and 2 add up to 4. And the unknown in medicine and life makes it worth seeking and living.
Introduction to Embryo Grading in IVF
Embryo grading is a key component of IVF treatment that helps assess the quality of embryos produced after the fertilization process in the IVF Lab. Embryologists evaluate embryos at various developmental stages to predict their chances of successful implantation and pregnancy. Grading of embryos allows an embryologist to select the most viable embryo for embryo transfer. This enhances the likelihood of a successful IVF outcome and often reduces the time to pregnancy. Understanding embryo grading can give patients valuable insight into the process of embryo selection and its impact on IVF success.
What Is Embryo Grading?
Embryo grading is the system used by fertility specialists to assess and classify embryos based on their developmental potential. The embryo grading scale considers various factors such as cell number, symmetry, and fragmentation to determine the embryo quality. High-quality embryos have a higher chance of successful implantation, leading to pregnancy.
By grading embryos at specific stages, embryologists can select the embryos with the highest likelihood of success during an embryo transfer.
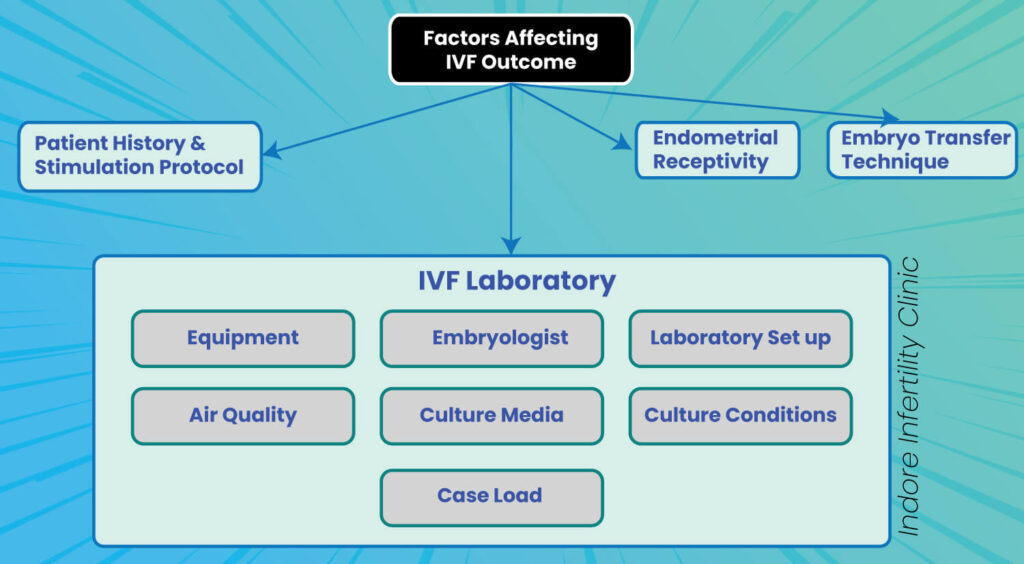
What are the factors that influence the quality of an embryo and hence embryo grade ?
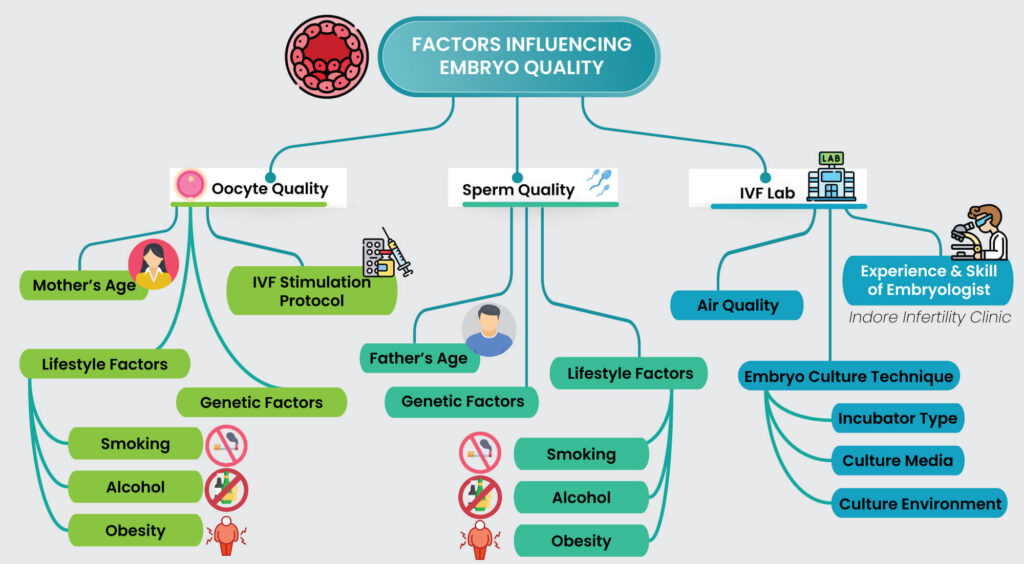
The factors influencing embryo quality can be categorized into 3 major components:
Oocyte Quality, Sperm Quality and IVF Lab Environment.
Here’s a detailed explanation based on the illustration:
Factors contributing to Oocyte Quality are
- Age of the Woman: Older women often have lower-quality oocytes due to reduced mitochondrial function and chromosomal abnormalities.
- Stimulation Protocol: Over or under stimulation or suboptimal protocols can affect oocyte maturity and quality.
- Lifestyle Factors: Smoking, obesity, and poor nutrition can impact oocyte health.
- Smoking – Smoking accelerates ovarian aging, reduces ovarian reserve, increases oxidative stress on ovum, damages oocyte DNA and reduces IVF success rates.
- Alcohol consumption – Excessive alcohol disrupts hormonal balance, impairing follicle development and ovulation, leading to poor egg quality and reduced IVF pregnancy rates.
- Obesity – Obesity leads to hormonal imbalances like insulin resistance and elevated androgens, impairing follicular development. It is linked to poor ovarian stimulation response, reduced egg quality, higher miscarriage rates, and an increased risk of chromosomal abnormalities in oocytes.
Factors impacting Sperm Quality
- Father’s Age: Advanced paternal age can affect sperm quality.
- Lifestyle Factors:
- Smoking – Smoking negatively impacts sperm quality by reducing sperm count, motility, and morphology, while increasing DNA fragmentation, which can impair fertilization and embryo development. Additionally, harmful chemicals in cigarettes lower testosterone levels, further hindering sperm production.
- Alcohol consumption – Alcohol disrupts spermatogenesis by altering hormone levels like testosterone, leading to reduced sperm concentration, motility, and viability. It also causes oxidative stress, damaging sperm DNA integrity.
- Obesity – Obesity lowers testosterone levels, reducing sperm production, motility, and increasing DNA fragmentation.
- Genetic Factors: Certain genetic conditions or predispositions may impact sperm quality.
IVF Lab Environment
- Air Quality: Clean and controlled air quality within the lab is critical for optimal embryo development.
- Embryo Culture Technique:
- Incubator Type: Benchtop incubators provide a stable environment for embryo development that is very close to what our body provides.
- Culture Media: The quality and composition of the media used play a significant role in embryo growth.
- Culture Environment: Maintaining the right temperature, pH, and humidity levels is crucial.
Experience & Skill of Embryologist: The expertise and precision of the embryologist greatly influence the handling and development of embryos. Accurate handling of gametes and skill during ICSI and embryo culture directly influence embryo quality.

Why Is it important to assess Embryo Quality ?
Embryo quality assessment is crucial in IVF because it directly impacts the success rates of implantation and pregnancy. High-quality embryos are more likely to implant in the uterus and lead to a successful pregnancy. While embryo quality isn’t the only factor influencing IVF success, it plays a significant role in the decision-making process of selecting the most viable embryos for embryo transfer.
Understanding the Embryo Grading Scale
The embryo grading scale depends on the day the embryos were graded or assessed. Typically, embryo grading is done at predefined time points during embryo culture.
Following are the grading systems based on the day of embryo transfer.
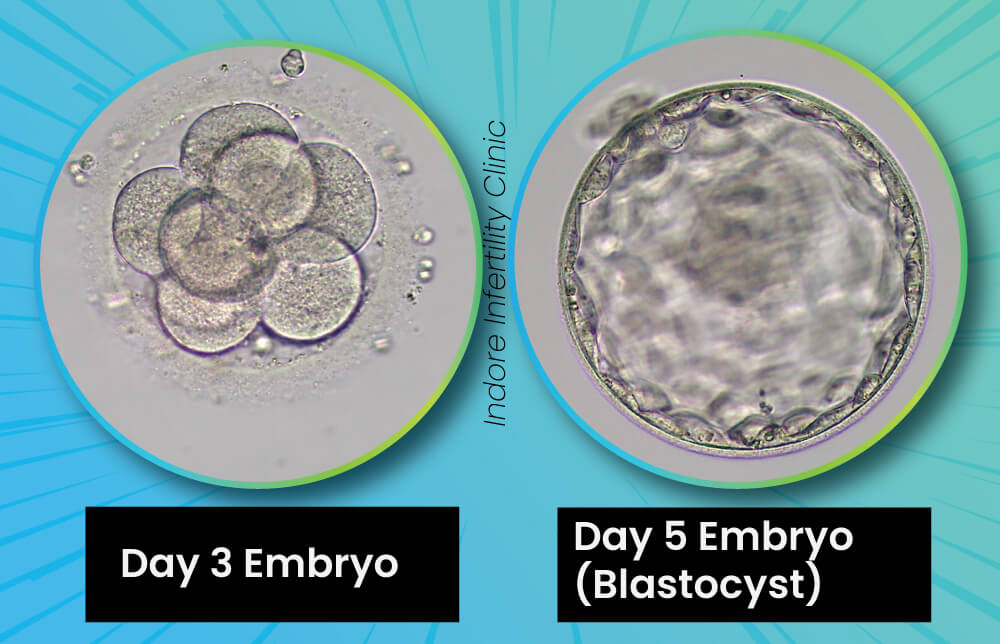
Day 3 Embryo Grading: Cleavage Stage Embryos
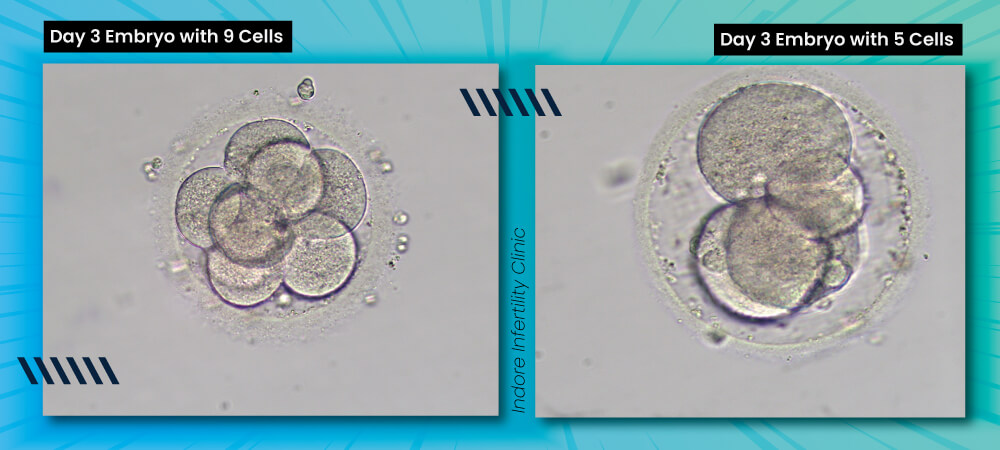
On Day 3 of embryo development, embryos are at the cleavage stage, typically consisting of 6 to 10 cells. Embryologists grade embryos at this stage based on the number of cells, their symmetry, and the amount of fragmentation present. Ideally, embryos should have equal-sized cells and minimal fragmentation, indicating better developmental potential.
Day 3 embryo grading helps determine which embryos are most likely to progress to the blastocyst stage and have the best chance of implantation during IVF.
Most clinics follow a standard way of grading cleavage stage embryos, the most followed cleavage stage embryo grading document is the Istanbul consensus on Embryo Assessment, which recently got updated in 2024.
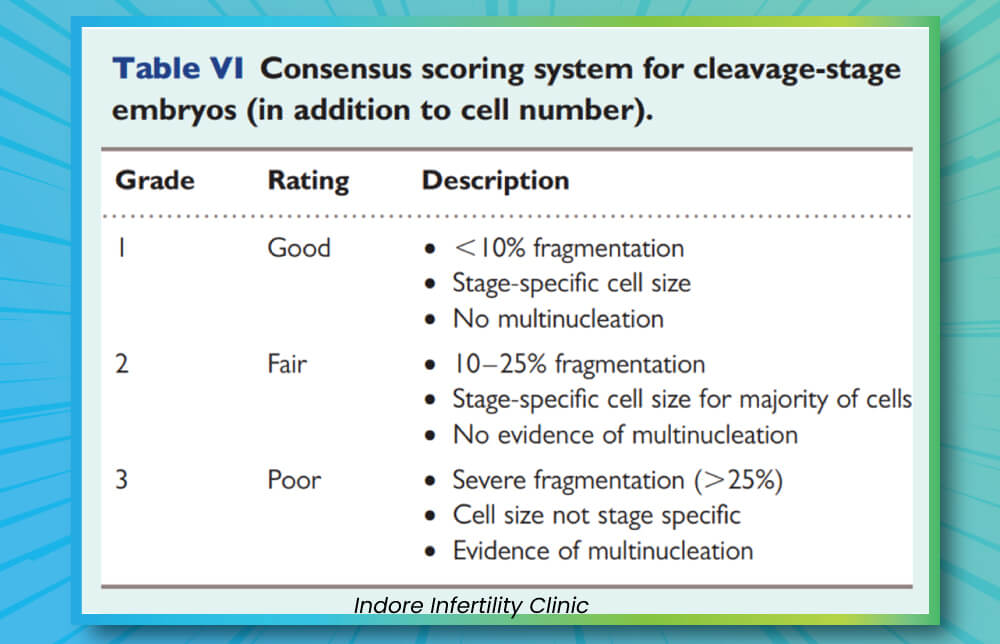
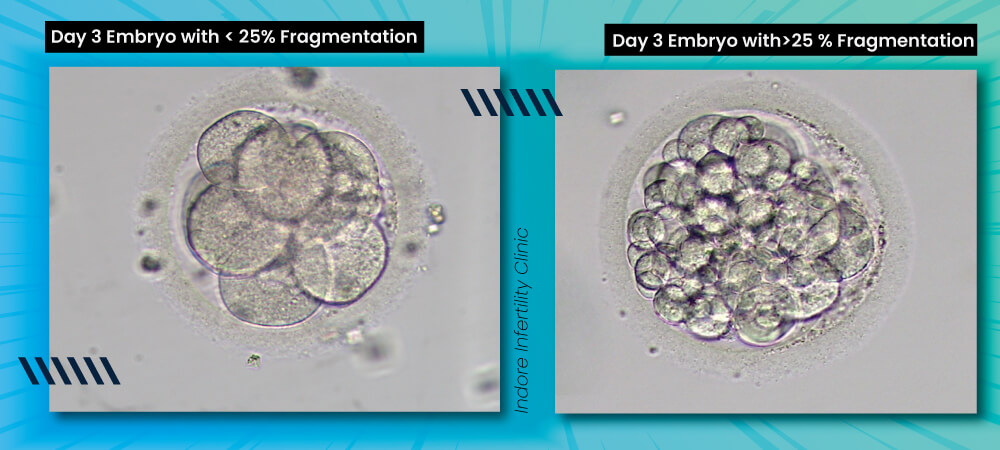
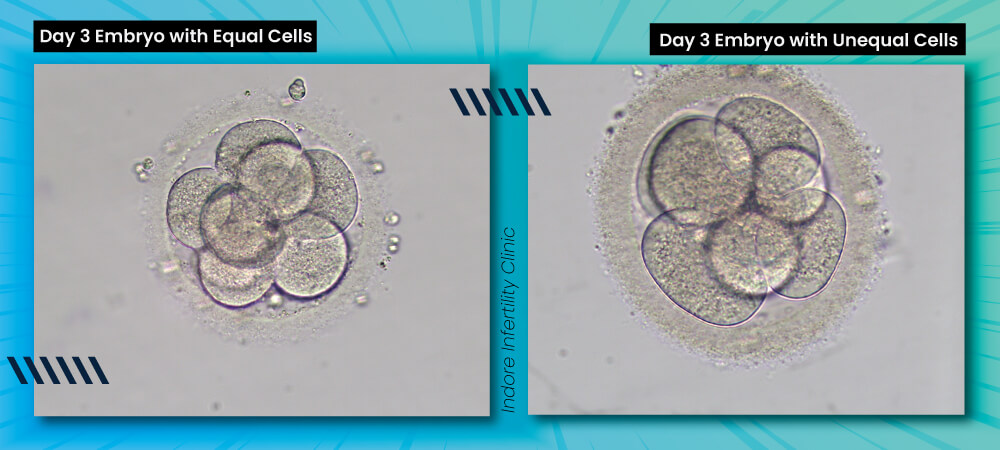
On Day 3, embryos are graded based on how many cells they have, their size, and the amount of fragmentation (small pieces of cytoplasm that break off during cell division).
Number of Cells: By Day 3, a healthy embryo typically has 6-10 cells. Embryos with fewer or significantly more cells may have a lower chance of developing into a blastocyst.
Cell Size: The cells should ideally be of equal size. Uneven cell sizes may indicate irregular division and could affect embryo quality.
Fragmentation: This refers to small fragments within the embryo that are not part of the cells. A low level of fragmentation is considered normal, but higher levels might reduce the embryo’s chances of implantation.
An embryologist will use this grading, along with other factors, to select the best embryos for transfer or freezing.
Day 5 Embryo Grading: Blastocyst Stage Embryos
By Day 5, embryos reach the blastocyst stage, characterized by the formation of a fluid-filled cavity called blastocoel. At this stage, embryologists grade embryos based on the quality of the inner cell mass (ICM), which will develop into the fetus, and the trophectoderm (TE), which will form the placenta. A well-defined ICM and a uniform TE indicate a high-quality blastocyst, which has the best chances of implantation and a successful pregnancy. Day 5 embryo grading is critical for selecting the most viable embryos for embryo transfer.
Blastocyst Grading system that is most frequently followed worldwide is the Gardner System of grading that associates an alpha numeric grade to a blastocyst. The Istanbul consensus is a slightly modified version of the Gardner grading system.
In order to understand a Blastocyst grading, we need to first understand the basic structure and parts of Blastocyst.
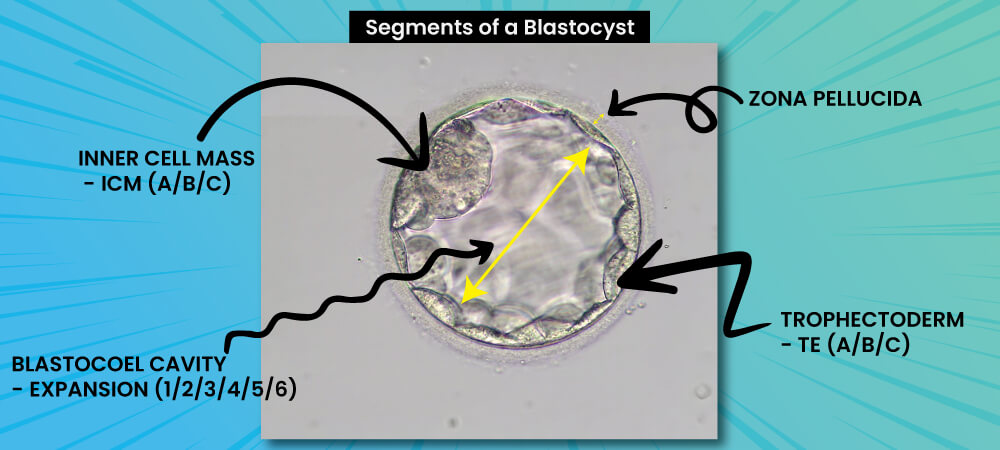
The Gardner scoring system for embryo grading was introduced by Prof. David Gardner in 1999. It is widely used for assessing the quality of blastocyst stage embryos in IVF. The system grades the embryo on three main components: blastocoel expansion, inner cell mass (ICM) quality, and trophectoderm (TE) quality. This scoring system helps embryologists predict the potential for implantation and pregnancy outcomes by evaluating these factors. The scale ranges from 1 to 6 for blastocoel expansion, and A to C for both ICM and TE quality.
Gardner Score for Blastocyst Grading
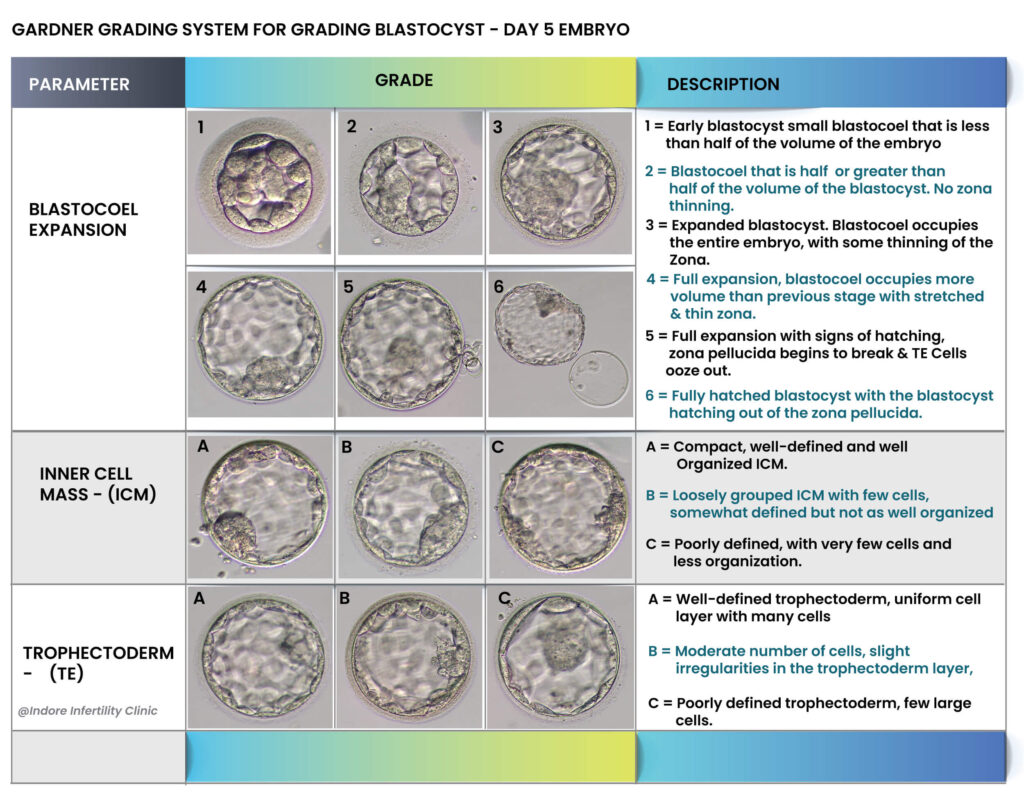
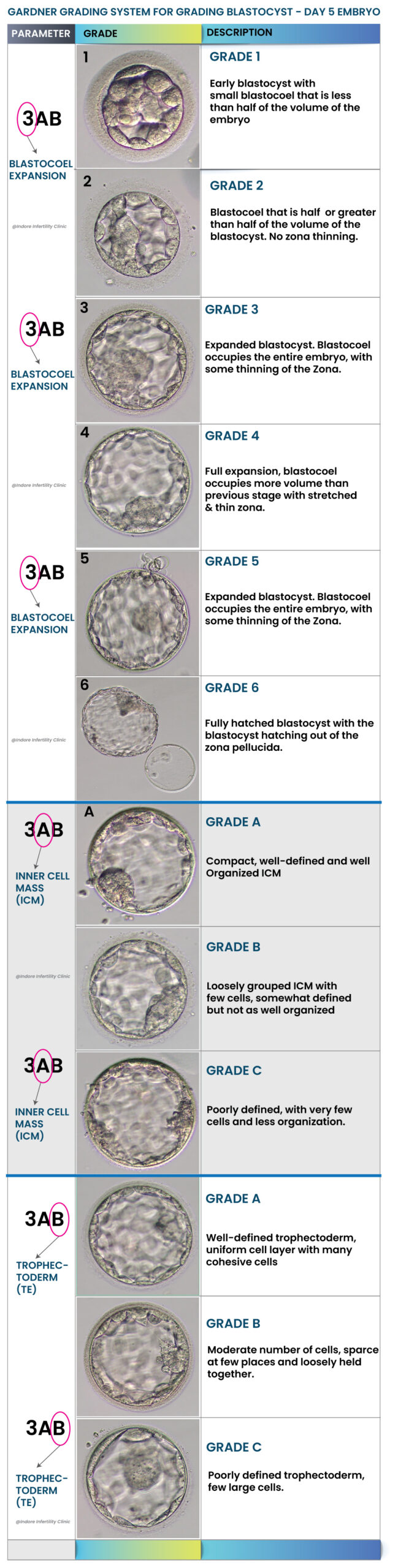
Factors Considered during Embryo Evaluation
Several factors are considered during embryo evaluation to determine the embryo’s quality:
- Cell number and symmetry: Embryos should ideally have cells that are similar in size, indicating proper division.
- Fragmentation: Excessive fragmentation is a sign of poor embryo quality. Minimal to no fragmentation is preferred.
- Developmental stage: The stage of development, whether cleavage or blastocyst, is a key factor during embryo assessment.
- Inner cell mass (ICM) and trophectoderm (TE): In blastocyst-stage embryos, the ICM and TE are critical for implantation and the formation of the fetus and placenta.
- Timing of Embryo assessment: Timing of embryo assessment is very important. Grade of an embryo is a variable that is associated to the morphology of the embryo, but missing the timeline of development, often referred as morphokinetics of embryo, makes the embryo less viable. In simple words a Good Blastocyst on Day6 is less viable than a good blastocyst on Day5.
Embryo Grading and IVF Success Rates
There is a direct correlation between embryo grading and IVF success rates. Higher-grade embryos, such as 5AA blastocysts, are more likely to implant and lead to a successful IVF pregnancy. However, while embryo quality plays a significant role, it is not the only factor influencing IVF success. Age, uterine health, and maternal as well as paternal factors also contribute to the chances of a successful outcome. Even lower-grade embryos may occasionally result in pregnancy, though they generally have a lower chance of success. Embryo grading helps prioritize the best embryos for embryo transfer so that eventually it reduces the time taken to pregnancy, often termed as TTP – Time to Pregnancy.
Limitations of Embryo Grading
Although embryo grading provides valuable insights, it is not a foolproof predictor of IVF success. The grading system can vary slightly between clinics, and some lower-grade embryos may still result in pregnancy despite their initial grading. Several other factors, such as the uterine environment, genetic and epigenetic factors, and maternal health, influence the success of implantation and therefore a pregnancy. Additionally, grading systems can vary between clinics and embryologists, leading to slight differences in interpretation.
Another important fact is that the current way of grading embryo at most clinics that lack timelapse incubator, is based on assessment of how the embryo looks at certain predefined timepoints, it does not take the entire journey of the embryo into consideration nor does it have insights to the metabolic profile or what each cell of the embryo intakes or releases. It is just a way of assessment of a physical appearance. Advancement in ART is coming up with much robust systems of embryo assessment like Timelapse incubators, AI models for embryo morphokinetics and metabolomic profile. Until these technologies are affordable and accurate enough, we will unfortunately have to stick to the traditional way of embryo grading.
Therefore, embryo grading should be viewed as a helpful tool in embryo selection but not the sole factor in determining IVF outcomes.
FAQ
FAQ's
Please go through the Blastocyst Grading section above to understand how Blastocysts’ are graded and what is the significance of the nomenclature. As explained above, the Blastocyst grade indicates the quality of the blastocyst by providing an objective score to the Blastocyst expansion, quality of ICM and TE.
Yes. For a specific cell stage. In short, for Day 3 or cleavage stage embryos, a Grade A Day 3 embryo should typically perform better than a Grade B embryo. Same for Blastocyst or Day 5 Embryo. Typically, a Grade 5AA Blastocyst on day 5 should perform better than a Grade 5AA Blastocyst on Day 6.
Yes absolutely. Embryology is medicine and not math. There is NO way for any embryologist to say with 100% surety which embryo will result in pregnancy and which will not. Embryologist can only predict based on knowledge from scientific literature and experience and yes predictions can go wrong too.

Embryologists in most IVF Labs, will remove the embryo culture dish in which embryos are being incubated from an Incubator, place the dish carefully under a inverted microscope, and quickly capture the required image after vidualizing the embryo under the microscope.
This is done very quickly usually under 30 seconds so that embryos are not harmed by fluctuations in the culture environment.
It is important to note that more experienced the embryologist, the lesser time they will take to perform these steps.
Embryo grades are assigned as per the stage of the embryo as explained in sections above.
A very crucial question, with a very crucial response. They say there are more than 200 variables that influence the outcome of an IVF cycle. The main entity that decides the fate of an IVF cycle is the embryo itself, which is formed by fertilizing the egg with a sperm.
Embryo quality and grade during IVF are influenced by several factors as explained in the sections above. Please do remember that not all parameters can be controlled. Some parameters are intrinsic, meaning internal to our body however, certain parameters can be influenced by making better choices.
Expertise of Embryologist
Accurate handling of gametes and skill during ICSI and embryo culture directly influence
embryo quality.
Embryo grading does not directly predict genetic health or abnormalities. While embryo grading assesses the morphological quality of embryos based on visual characteristics such as blastocyst expansion, inner cell mass (ICM), and trophectoderm (TE), it does not reveal the chromosomal or genetic status of the embryo. However, there are studies that mention that a morphologically better looking embryo does have higher chances of being chromosomally normal as compared to poor looking embryo.
As explained above, Day 3 or Cleavage stage embryo have a different grading style as compared to Day 5 or Blastocyst stage embryos.
Yes, lifestyle change can definitely improve quality of eggs and sperm over months, and hence they do have a potential to improve embryo quality. Better quality embryo will have better embryo grading.
Only growing embryos are graded, i.e. on Day 5, if there are 3 Blastocyst and rest of the embryos did not progress to Blastocyst stage, then embryologist will only grade the 3 growing blastocyst and the rest of the embryos will be discarded.
In such a case, the Infertility specialist will counsel you towards the expected outcome and leave the decision of transferring low grade embryos to you. As explained before, it is not currently possible to just look at an embryo and say if it has potential to implant and result in a live birth. So, if you do not have any high grade embryo, you should still go ahead and get the best of the lot transferred. Let nature take it’s course.
Depends. The word poor is very subjective. For patients with poor ovarian reserve where future IVF cycle with chances of making better embryos, is not a practical option, then poor quality embryos (lower grade, but stage specific embryos meaning embryos that have reached that stage on Day 3 or Day 5) can be frozen for taking a chance. However, please note that the process of freezing and warming might impact the quality further.
Yes, all the time. Embryo grading currently is a very subjective process. Even if two embryologist follow the same guideline, they end up grading an embryo differently, especially in borderline cases. Clear cut good or bad embryos, typically are graded similarly by embryologist.
Embryos with fragmentation will be graded lower than embryos without fragmentation. Please read the above paragraphs on Cleavage stage embryo grading to understand better.
Embryo grading is a useful tool in IVF, but its accuracy in predicting outcomes is limited and not absolute. Higher-grade embryos (e.g., Grade A or 5AA blastocysts) are more likely to implant as compared to lower grade embryos. Studies have proven that morphological assessment usually correlate to higher implantation rate. Good grades indicate better structural quality, which often translates to higher survival rates after freezing or transfer.
No Guarantee of Success:
- High-grade embryos can still fail to implant due to factors like uterine environment, endometrial receptivity, or genetic abnormalities.
- Conversely, lower-grade embryos sometimes result in successful pregnancies.
Yes, an embryo’s grade can change as it develops. Embryo grading is a dynamic process, and changes can occur as the embryo progresses through different stages of development.
Factors Influencing Grade Changes
- Embryo's Intrinsic Quality: Genetic and cellular factors significantly influence development and grade changes.
- Culture Conditions: Suboptimal lab conditions can negatively affect embryo morphology, while ideal conditions may support improvement.
- Autocorrection by Embryos:
Embryos have an innate ability to autocorrect certain developmental abnormalities. For example:
Chromosomal Mosaicism: Embryos may eliminate abnormal cells through mechanisms like apoptosis (programmed cell death), leading to an improved overall quality.
Fragment Reabsorption: During early stages, embryos can reabsorb fragments or redistribute cellular contents, improving their appearance and grade.
Reorganization of Cell Structures: Blastocysts, for instance, can reorganize their inner cell mass (ICM) and trophectoderm (TE), leading to better-defined and higher-grade structures over time.
Yes, embryo grading plays a crucial role in deciding whether to transfer one or more embryos during IVF. While high-grade embryos encourage single embryo transfer, lower grades may lead to multiple embryo transfers to statistically enhance success rates. The ultimate decision balances the embryo's grade, patient factors, and clinical goals for a healthy singleton pregnancy.
None actually. Embryo grade decides the order of embryo during embryo transfer. There is no other factor other than the embryo grading, that might impact the decision of transferring one embryo over the other.
When an embryo is graded as "fair" or "poor," it refers to the quality of the embryo based on its developmental stage, cell appearance, and structure. These grades are not definitive predictors of success but are used by embryologists to make informed decisions about which embryos to transfer.
No.

Yes, Indirectly. Grading in itself does not, but as explained before, when most of the embryos are graded moderate to poor, clinician may transfer more than one embryo to statistically improve the chances of implantation. And transferring two or more embryos will lead to increases chances of having twins.
Also, in some rare cases, a single embryo might go ahead to develop into a monozygotic twin. It is however currently not possible to identify which embryo will develop into a monozygotic twin by mere morphological assessment of the same.
The inner cell mass (ICM) is a crucial component of the blastocyst or Day 5 embryo. It consists of a cluster of cells that will eventually develop into the fetus. A well-formed, compact ICM is a sign of a healthy, high-quality embryo, which has better potential for implantation and successful pregnancy. The size and structure of the ICM are closely observed during grading. A larger, well-organized ICM is typically associated with a higher likelihood of successful outcomes. ICM quality is graded with letters A, B and C where A is the best grade.
The trophectoderm is the outer layer of cells in the blastocyst that will ultimately form the placenta. Its quality plays a critical role in both embryo grading and implantation success
The trophectoderm's quality is assessed based on the uniformity, size, and structure of its cells. High-quality trophectoderm cells are typically tightly packed, with minimal fragmentation and clear, distinct borders.
Trophectoderm grading is usually scored on a scale (e.g., A, B, C) based on the number of cells, degree of fragmentation, and overall cohesiveness.
The trophectoderm is responsible for forming the placenta, which provides nutrients and support to the developing embryo.
A high-quality trophectoderm enhances the embryo's ability to attach to and invade the uterine lining, fostering proper implantation.
Poor-quality trophectoderm may impair the embryo's ability to effectively implant, leading to a higher risk of implantation failure.
Several technologies are employed in embryo grading to assess the quality and developmental potential of embryos. These include both traditional and advanced techniques: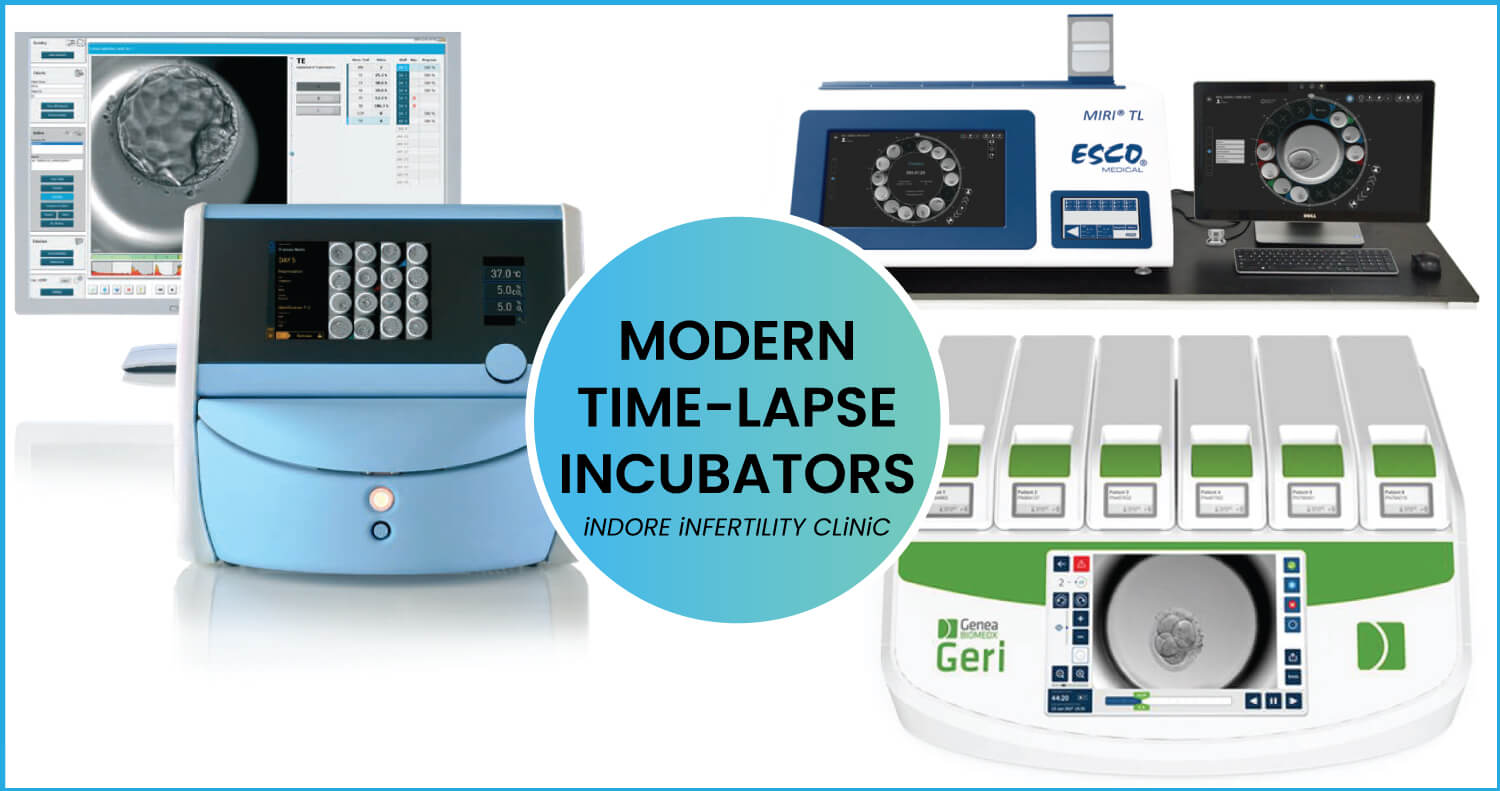
Light Microscopy: Traditional tools for Embryo Assessment
Embryologists use phase contrast or differential interference contrast (DIC) microscopy to observe embryos at various stages of development.
Time-Lapse Imaging: Advance Techniques
A specialized incubator with built-in cameras that capture images of embryos continuously over a period (typically 3-6 days).
Provides detailed information about embryo development, including timing of cell
divisions, embryo morphology, and any irregularities, all without disturbing the culture
environment of the embryos.
Preimplantation Genetic Testing (PGT): Invasive Assessment of Embryos
- PGT-A (Aneuploidy): Detects chromosomal abnormalities in embryos (e.g., Down syndrome).
- PGT-M (Monogenic disorders): Screens for single-gene disorders.
- PGT-SR (Structural Rearrangements): Detects structural chromosome issues.
- Impact on Grading: Embryos with normal genetic profiles (from PGT) are more likely to be selected for transfer.
Artificial Intelligence (AI) Tools:
- AI-based Embryo Assessment: AI algorithms analyze images from time-lapse systems or static images captured by microscope to predict embryo viability by recognizing patterns associated with successful implantation.
- Deep Learning: AI models are trained on large datasets of embryo images to make predictions on embryo quality and success rates, assisting embryologists in grading.
Non-invasive Metabolomics:
- Metabolic Profiling: Measures the metabolic activity of embryos to predict viability.
- Techniques: Mass spectrometry or nuclear magnetic resonance (NMR) spectroscopy can be used to analyze metabolites in culture media, offering insights into embryo health.
In summary, modern embryo grading combines traditional microscopy with cutting-edge technologies like time-lapse imaging, AI tools, and genetic testing to provide more accurate and comprehensive evaluations of embryo quality and implantation potential.
No. Embryo grading alone cannot directly detect chromosomal abnormalities. Grading primarily evaluates the morphological quality of an embryo. However, grading does not assess the genetic makeup of the embryo. To detect chromosomal abnormalities, specialized genetic testing like PGT-A is required. PGT is typically performed on embryos by taking a biopsy (removing a few cells) after reaching the blastocyst stage and analyzing the DNA of those cells for any abnormality in genetic labs. Grading focuses on physical and developmental characteristics of the embryo, while PGT evaluates its genetic and chromosomal health.
Maternal age has a significant impact on both embryo quality and grading. As women age, particularly after the age of 35, the quantity and quality of their eggs decline, leading to several changes in embryo development and grading. Older women are more likely to produce embryos with chromosomal abnormalities, delayed development, and higher fragmentation, which in turn results in lower embryo grades.
Embryos from older women often receive lower grades due to irregular cell division, high fragmentation, and incomplete or poor development.
As maternal age increases, the likelihood of genetic abnormalities in embryos also increases.
Even though two embryos may have the same grade, there can still be differences in their implantation outcomes due to several factors that are not fully captured by grading systems.
Here are some reasons why this might happen:
- Genetic Factors (Chromosomal Health):
Grading primarily evaluates the morphological quality of the embryo, not its genetic integrity. Two embryos with similar grades could have very different genetic profiles.
One embryo might be chromosomally normal (euploid), while the other could have chromosomal abnormalities (aneuploidy), leading to a lower chance of implantation and a higher risk of miscarriage.
- Embryo Epigenetics:
Epigenetic factors, which affect gene expression without changing the DNA sequence, can influence how embryos implant and develop. In simple words epigenetics are how genes function in the immediate environment, i.e. even though two cells may have same genetic code, minor changes in environmental factors around the cells make the genes behave differently. These factors are not assessed by grading systems.
- Embryo-Maternal Interaction:
Successful implantation depends on the interaction between the embryo and the uterine lining (endometrium). Even if embryos are graded similarly, their ability to adhere and invade the endometrium might vary due to subtle differences in trophectoderm quality or molecular signalling.
Factors like endometrial receptivity or immunological environment may play a role in the embryo's ability to successfully implant.
- Timing of Implantation:
The timing at which embryos are transferred can influence their implantation potential. Even embryos of the same grade may behave differently depending on whether they are transferred within the implantation window or not.
- Embryo Handling during Embryo Transfer:
Differences in the way embryos are handled during the embryo transfer process by an embryologist & clinician can also affect their development and implantation success. The aim should be to make the embryo transfer as atraumatic as possible.
- Uterine Factors:
Factors such as the endometrial lining thickness, hormonal environment, and presence of fibroids or polyps can all impact implantation success.
Even embryos with identical grades can have different outcomes based on how well the uterus is prepared for implantation.
Summary:
Grading is an important tool for assessing embryo quality, but it does not capture the full picture of an embryo's potential for implantation. Factors like genetic health, epigenetics, embryo-maternal interactions, and uterine conditions all play critical roles in determining whether an embryo will implant successfully, even if two embryos have the same grade.
Absolutely, the experience of the embryologist can significantly impact the accuracy of embryo grading. Experienced embryologists tend to have a better understanding of subtle morphological differences between embryos, which can improve consistency and precision in grading. Their familiarity with the embryonic development and grading protocols helps them assess embryos more effectively. However, despite experience, human bias and subjectivity can still influence grading, which is why some centre’s are adopting AI-based tools for embryo grading to standardize the process and reduce inter-observer variability.
No. Embryos do not improve in quality after being cultured longer, but their developmental potential may become clearer with time. Extended culture allows embryos to reach the blastocyst stage, where their viability can be more accurately assessed based on additional parameters like trophectoderm and inner cell mass development. However, extended culture should only be used as a selection technique to select the best from the lot. Hence, when one has only one or two embryos, extended culture does not always make sense.
Artificial intelligence (AI) plays a transformative role in embryo grading by improving accuracy, consistency, and efficiency of the embryo grading process:
- Standardization: AI eliminates inter- and intra-observer variability by applying consistent algorithms for grading embryos. Meaning, AI tools will always grade an embryo consistently unlike embryologist, who often end up grading the same embryos differently when presented in different times.
- Image Analysis: AI analyzes static images or time-lapse videos to assess morphological and dynamic developmental patterns that may be too subtle for human observation.
- Predictive Insights: By correlating image features with known outcomes of thousands of images/videos (e.g., implantation, pregnancy), AI algorithms predict the implantation potential and viability of embryos more accurately as compared to embryologist, who have limited exposure to embryo and outcome based on their experience.
- Time Efficiency: AI tools reduce the time needed for manual grading, allowing embryologists to focus on other critical tasks.
- Better Reporting: AI Tools have capability to automate the embryo grade reporting enhancing the patient experience.
- Learning and Adaptation: AI systems improve over time through machine learning, becoming increasingly reliable as they process larger datasets.
AI-assisted embryo grading complements the expertise of embryologists, helping to optimize embryo selection and enhance patient experience.
Embryo grading plays a crucial role in decisions regarding preimplantation genetic testing (PGT) by helping identify embryos most suitable for testing and transfer.
- Selection for Biopsy: Embryos with good morphology and development are prioritized for biopsy since they are more likely to survive the procedure and yield reliable genetic results.
- Cost Efficiency: Grading helps avoid unnecessary testing of poor-quality embryos that are less likely to result in successful pregnancy, optimizing resource use.
- Avoiding Damage: Poorly graded embryos may be more fragile, increasing the risk of damage during biopsy, making grading an important screening tool before biopsy.
- Improved Outcomes: High-grade embryos with normal genetic profiles (euploid) have higher implantation and live birth rates, enhancing the efficiency of IVF cycles.
While embryo grading guides PGT decisions, it does not guarantee genetic normalcy. Combining grading with PGT provides a more comprehensive assessment of an embryo’s potential.
It is important to note that decision on whether you want to opt for PGT should be discussed with clinician before your ovum pickup. PGT often involves high cost and logistical considerations with regards to sending the biopsied cells to genetic lab in timely and safe manner. Deciding to biopsy embryos on Day 5 suddenly will cause a lot of unwarranted chaos in the IVF Lab and hence usually not done in standard IVF Clinics.
No, embryos with the same grade do not necessarily have equal chances of success in fresh vs. frozen transfers. The success rates depend on several factors beyond the embryo grade, including the uterine environment and hormonal conditions. Here's how the two scenarios differ:
Fresh Transfers:
Fresh transfers may be affected by the ovarian stimulation drugs used, which can reduce uterine receptivity. As a result, implantation rates might be lower compared to frozen transfers, even when the embryo grade is the same.
Frozen Transfers:
Frozen transfers benefit from a controlled, hormone-optimized environment that improves uterine receptivity. Vitrification technology preserves the quality of the embryos, and modern thawing techniques ensure high survival rates.
While high-grade embryos generally perform well in both transfer types, frozen embryo transfers (FET) often yield better outcomes due to improved synchronization between the embryo and endometrium.
Yes, embryo grading can be influenced by the ovarian stimulation protocol used in IVF, as the quality of oocytes retrieved and the resulting embryos can be affected by hormonal levels and ovarian response. Here's how:
- Oocyte Quality:
- High doses of gonadotropins (Injections used during IVF Stimulation process) in some protocols may lead to oocyte retrieval from follicles at different maturation stages, potentially affecting embryo development and quality.
- Mild stimulation protocols may yield fewer, but often higher-quality oocytes, leading to better-quality embryos.
- Hormonal Environment:
- Excessive estrogen levels or suboptimal luteal support from certain protocols can indirectly affect embryo quality and grading by impacting oocyte maturation.
- Cumulative Impact:
- Suboptimal protocols might lead to suboptimal oocytes which may result in impaired embryo development, impacting morphology and the resulting grades.
Selecting an individualized stimulation protocol is essential to optimize oocyte quality and, consequently, embryo grading and IVF outcomes.
Yes, it could have. Embryo quality significantly impacts IVF success, as lower-grade embryos often have reduced implantation potential and a higher likelihood of genetic abnormalities, leading to failure or miscarriage. However, IVF failure is multifactorial, influenced by factors like uterine receptivity, hormonal imbalances, and embryo transfer technique. In cases of multiple IVF failures, advanced tests such as genetic evaluations, uterine assessments, and immunological testing for NK cell activity can help identify underlying causes.
Since no two oocytes and sperms are same, no two embryos are exactly the same.
Embryos from the same IVF cycle can be graded differently due to variations in oocyte quality, sperm contribution, and culture conditions, such as nutrient uptake or pH differences. These factors affect individual embryo development, making grading variability normal. Embryologists prioritize selecting the best-quality embryos for transfer or freezing.
Embryos with fragmentation generally have a lower chance of success as it can impair cell division, reduce implantation potential, and is often associated with chromosomal abnormalities. Significant fragmentation disrupts development, but mild fragmentation (under 20%) is common and may not greatly affect viability. Advanced grading and imaging techniques help assess their potential more accurately.
If your embryos stopped growing after Day 3 and did not reach the blastocyst stage, it typically indicates that the embryos lacked the necessary developmental potential. This could be due to factors like poor oocyte or sperm quality, genetic abnormalities, or suboptimal culture conditions in the IVF Lab. Some embryos may arrest early in development, failing to progress beyond certain stages due to inherent limitations in their biology. It's important to discuss with your embryologist to understand possible underlying causes and explore options for future cycles.
Blastocysts on Day 5 are generally considered better than those on Day 6 of development, even if they are of the same grade. This is because embryos that reach the blastocyst stage on Day 5 are typically more developmentally advanced, suggesting better overall quality and higher implantation potential. However, some embryos may naturally require an extra day to fully develop, and a Day 6 blastocyst can still have strong implantation potential, especially if it's of high quality. The key is the embryo's developmental progression and morphology, not just the day it reaches blastocyst stage.
While poor-quality embryos have a lower chance of implantation and pregnancy success, it is still possible for them to implant and lead to a healthy baby. In some cases, embryos with minor imperfections or lower grades may still possess sufficient developmental potential and genetic integrity for a successful pregnancy. Embryos have a concept known as "autocorrection," where they can sometimes compensate for minor issues during early development, leading to healthy outcomes. However, the likelihood of success is lower compared to high-quality embryos, and factors such as uterine receptivity and overall health of the embryo also play a crucial role. It's important to remember that each embryo is unique, and the outcome can vary.
"Arrested development" in embryos means that their growth has stopped at a certain stage and they fail to progress further. This can happen for various reasons, such as poor oocyte or sperm quality, genetic abnormalities, or unfavorable culture conditions.
Embryos with arrested development often fail to reach critical stages like the blastocyst stage and are unlikely to result in a successful pregnancy.
Yes, the IVF lab's conditions can affect embryo grading. Factors like temperature fluctuations, pH levels, nutrient supply, air quality in IVF lab and the culture medium can influence embryo development. Even small variations in these conditions can impact embryo growth, morphology, and overall quality. Additionally, handling techniques and the timing of embryo assessments also play a role in grading. A well-controlled, optimized IVF lab environment is crucial for maximizing embryo quality and grading consistency.
An embryology report can provide insights into potential issues with egg or sperm quality based on factors like fertilization rates, embryo development, and morphology. If there are low fertilization rates, poor embryo quality, or slow development, it may suggest concerns with egg or sperm quality. For example, low embryo quality might indicate poor oocyte quality or sperm with genetic abnormalities. However, a detailed analysis of the fertilization process, embryo progression, and grading will help identify specific issues. It's important to discuss the report with your embryologist for a more tailored interpretation based on your individual case.
Yes, embryos with lower grades are generally less likely to survive the freezing and thawing process compared to higher-grade embryos. Poorer-quality embryos often have less robust cell structure, which can make them more vulnerable to damage during cryopreservation. Factors like cell fragmentation or irregular morphology can affect their ability to survive the freezing and warming process. However, advancements in vitrification technology have improved the survival rates of embryos, even those with moderate quality, though high-quality embryos still tend to fare better in this regard.
When embryo grades are low in an IVF cycle, it’s important to investigate the underlying cause. An experienced embryologist can help assess whether the low grading is due to the inherent quality of the oocytes or eggs, or if lab conditions or the stimulation protocol might be contributing factors. Since the same medication does not have a uniform response in all patients, trying a different stimulation protocol could be worthwhile. However, if multiple IVF cycles have failed with similar outcomes, there is a high probability of a genetic cause. In such cases, the couple should first undergo genetic testing. Since invasive procedures like embryo biopsy may not always succeed with poor-quality embryos, using donor gametes, such as donor eggs or sperm, might be a viable option to improve success chances.
To improve embryo quality in your next IVF cycle, consider these steps:
- Optimize Stimulation Protocol: Work with your doctor to tailor your ovarian stimulation protocol. Different medications and dosages can be more effective depending on your response, so adjusting the protocol could yield better results.
- Review Lifestyle Factors: Maintain a healthy lifestyle by eating a balanced diet, exercising regularly, and avoiding smoking, alcohol, and excessive caffeine. These factors can improve egg quality.
- Consider Supplements: Some studies suggest that supplements like Coenzyme Q10 (CoQ10), DHEA, or folic acid may improve egg quality, but consult with your doctor before starting any supplements.
- Hormonal Health: Consider evaluating hormonal levels, thyroid function.
- Consider Genetic Testing: In cases of multiple IVF failure, it might be advisable that patient undergoes genetic testing to see assess genetic competence.
- Embryo Culture and Handling: Ensure that your IVF lab uses the latest culture systems, experienced embryologist who can monitor and select the best embryos for transfer.
By taking these steps and discussing with your fertility specialist, you can optimize conditions for better embryo quality in your next cycle.
Yes, it's possible that embryos were graded too harshly or inaccurately, though experienced embryologists generally use standardized criteria for grading. Variations in grading can occur due to subjective interpretation or differences in embryologist experience, culture conditions, or even the timing of embryo evaluation. However, grading discrepancies are usually minimal, as labs strive for consistency. If you have concerns, discussing the grading process with your embryologist can provide clarity. In some cases, using advanced tools like AI based embryo assessment can offer a more objective and accurate assessment of embryo quality.
Embryo grading helps determine whether to opt for fresh or frozen embryo transfer by assessing embryo quality and developmental potential. High-quality embryos and an optimal uterine environment may favor fresh transfer, ensuring no delay in achieving pregnancy. However, if the uterine lining is suboptimal or there’s a need for preimplantation genetic testing, freezing allows for better timing and selection of the best embryo. Frozen transfers also provide flexibility for better synchronization with the uterine environment and receptivity potentially increasing the IVF success rates.
A failed IVF cycle doesn’t necessarily mean you should avoid transferring embryos with a similar grade in the future. Embryo grading is only one factor in predicting success, and other aspects like uterine receptivity, hormonal balance, and lab conditions also play a significant role. If the embryos were graded as good or fair, they might still have implantation potential. Discussing the specifics of your cycle with your doctor, including possible adjustments to the protocol, can help determine the best approach for future transfers.

Yes, poor-grade embryos may have a higher risk of miscarriage due to potential chromosomal abnormalities or suboptimal development. Studies have shown that embryos with a lower grade of trophectoderm, which forms the placenta, are associated with an increased risk of miscarriage. However, not all poor-grade embryos result in miscarriage, as some can still implant and lead to healthy pregnancies. Factors like uterine environment and hormonal support also play a significant role. Discussing embryo quality with your doctor can help assess risks and guide your next steps.
Yes, poor-grade embryos are more likely to result in biochemical pregnancies due to their reduced implantation potential and higher likelihood of chromosomal abnormalities. These embryos may begin the implantation process but fail to develop further, leading to an early pregnancy loss. However, not all poor-grade embryos result in biochemical pregnancies, as other factors like uterine receptivity and hormonal balance also influence outcomes.
Yes, poor-grade embryos generally have a higher chance of chromosomal abnormalities, as their suboptimal development may reflect issues in cell division or genetic integrity. Chromosomal abnormalities can reduce implantation potential and increase the risk of miscarriage. However, grading alone is not definitive, and testing such as preimplantation genetic testing (PGT) can provide more accurate information about the embryo's chromosomal status.
Yes, embryo grade could have contributed to your miscarriage or early pregnancy loss, especially if the embryo had poor morphology or a lower trophectoderm grade, which is associated with higher rates of chromosomal abnormalities and implantation failure. However, other factors such as uterine receptivity, hormonal imbalances, or immune issues might also have played a role.
To improve implantation chances with a lower-grade embryo, optimizing the uterine environment through hormonal support, and ensuring proper timing of embryo transfer are key. Timing the embryo transfer during a receptive window, often determined by the endometrial lining, is crucial. Addressing overall health, including lifestyle factors, further supports success. These strategies can maximize implantation chances, even with lower-grade embryos.
The uterine environment plays a critical role in the implantation of poor-grade embryos. Even if an embryo is of lower quality, a well-prepared uterine lining can significantly improve implantation chances. Factors like optimal endometrial thickness, hormonal balance (especially progesterone), and proper timing of embryo transfer are crucial. A receptive uterus increases the likelihood that the embryo, despite being of lower grade. Therefore, improving uterine conditions through hormonal support and an atraumatic embryo transfer procedure may enhance outcomes for poor-grade embryos.
Recent studies have shown mixed results regarding the effectiveness of assisted hatching in improving implantation rates for poor-quality embryos. While the technique was initially thought to help embryos with a thickened zona pellucida, recent literature suggests that it may not significantly enhance implantation or pregnancy outcomes. The benefits of assisted hatching likely depend on factors such as embryo quality and the uterine environment, meaning it may not be universally effective for all cases involving poor-quality embryos.
Yes, poor-grade embryos are more likely to stop growing after implantation due to potential chromosomal abnormalities or developmental issues. These embryos may struggle to develop properly after implantation, leading to early pregnancy loss or miscarriage. However, not all poor-grade embryos fail to progress, as some can still result in viable pregnancies. Factors like uterine receptivity, hormonal support, and overall embryo quality also play a significant role in the outcome.
Bleeding or spotting after embryo transfer can occur for various reasons and isn't necessarily a direct sign of poor implantation due to low-grade embryos. It may be caused by the embryo's implantation process or hormonal changes related to the IVF treatment. While poor-quality embryos may have a higher risk of implantation failure, light bleeding or spotting doesn't always correlate with embryo quality. It's important to monitor for other signs and consult with your doctor to assess the situation and determine if further evaluation or intervention is needed.
Yes, a high-grade embryo can still cause bleeding or spotting after embryo transfer. This may happen due to the implantation process, where the embryo embeds itself into the uterine lining, potentially causing light bleeding. Spotting can also occur due to hormonal fluctuations or the effects of medications used during the luteal phase of the IVF cycle. While it’s less likely to be associated with embryo quality, any bleeding or spotting should be monitored, and it’s important to consult with your doctor to rule out other potential causes and assess the situation.
Heavy bleeding after embryo transfer, even with a good-grade embryo, is a cause for concern and should be addressed promptly. It may indicate issues like uterine irritation, an ectopic pregnancy, or other complications that could affect implantation or pregnancy. While spotting can be common, heavy bleeding typically requires medical evaluation. It’s important to contact your IVF Specialist to assess the situation and determine whether further testing or intervention is needed.
Automation in embryo grading uses advanced imaging systems, artificial intelligence (AI), and machine learning algorithms to assess embryo quality more objectively and consistently. These systems analyze factors like cell morphology, symmetry, and developmental timing or embryo morphokinetics to assess embryos. Automation can process large amounts of data more efficiently than manual grading, reducing human bias and variability. While its use is growing, it’s not yet universally adopted, as many clinics still rely on expert embryologists for final grading. However, automation is becoming more common as the technology improves and proves its accuracy in predicting embryo viability.
AI shows promise in predicting embryo success by analyzing vast amounts of data from factors like embryo morphology, development patterns, and genetic information. AI algorithms, especially those using machine learning, can identify subtle patterns in embryo images that might be missed by human embryologist, potentially improving predictions of implantation and pregnancy success. However, while AI has demonstrated accuracy in some studies, it is not yet perfect and should be used in conjunction with expert clinical judgment. It is becoming an increasingly valuable tool, but it is not yet a definitive predictor of success in all cases.
AI-assisted grading systems have shown promising results in some studies, often outperforming manual grading by embryologists in terms of consistency and objectivity. AI can analyze large datasets quickly, reducing human error and variability. It can identify subtle patterns in embryo morphology and development that may be overlooked by human graders. However, while AI shows potential, it is not yet universally accepted as superior to manual grading. Many clinics still rely on embryologists for final assessments, as AI systems are not yet fully refined or universally applicable in all clinical settings.
AI tools can be reliable in grading embryos with fragmentation or other abnormalities, as they are designed to analyze and quantify subtle patterns and abnormalities that may be difficult for human embryologists to detect. AI algorithms can assess the extent of fragmentation, cell division, and other irregularities, helping to provide a more objective and consistent evaluation. However, while AI can be effective, its reliability may vary depending on the quality of the training data and the specific abnormalities. In cases of severe fragmentation or complex abnormalities, expert clinical judgment is still important to ensure accurate grading and decision-making.
AI can assist in detecting patterns associated with chromosomal abnormalities by analyzing morphology, development patterns, and other embryonic features. While AI alone cannot directly detect chromosomal issues like aneuploidy, it can help identify embryos with a higher likelihood of carrying abnormalities. This allows for better selection, potentially optimizing the number of embryos that need to be biopsied for Preimplantation Genetic Testing (PGT), which could reduce both the cost and the invasive procedures required. AI thus complements genetic testing, improving embryo selection and potentially act as a screening tool for choosing embryos that need to be biopsied.
AI tools have the potential to reduce the time to pregnancy by streamlining the process of embryo selection. By analyzing various factors like embryo morphology and development, AI tools can help identify embryos with the highest likelihood of success more efficiently. However, while AI shows promise, its full impact on IVF success rates is still being studied, and further research is needed to validate its effectiveness. It should be viewed as a decision support tool in embryo selection, rather than a guaranteed method for improving pregnancy outcomes.
AI tools cannot fully replace embryologists in assessing embryo quality. While AI can assist by providing objective and consistent evaluations of embryo morphology and development, embryologists bring essential expertise in interpreting complex factors, such as patient history and the broader clinical context. AI can be a valuable tool to support and enhance decision-making, but the expertise, judgment, and experience of embryologists remain crucial in ensuring that the reports generated upon by AI are interpreted accurately. AI should be seen as a complementary tool, not a replacement.
Yes, there can be differences in embryo grading results between AI systems and human embryologists. While AI systems provide consistent, data-driven evaluations based on predefined algorithms, human embryologists can consider a wider range of factors, including patient history, clinical context, and subtle visual cues that may not be captured by AI. However, AI systems are improving in accuracy and can help reduce variability in embryo grading, potentially complementing the work of embryologists rather than replacing them.
AI-based embryo grading tools are still relatively expensive for IVF clinics, especially for smaller IVF Clinics, due to the high costs associated with developing, implementing, and maintaining the technology. The price of AI systems varies depending on the complexity of the tool and the clinic's needs. While these tools have the potential to improve efficiency and reduce costs in the long run by optimizing embryo selection, the initial investment can be a barrier.
AI tools in embryo grading have several limitations. First, they rely heavily on the quality and quantity of data used to train the algorithms. If the data is incomplete or biased, the AI's accuracy can be compromised. Additionally, AI systems may struggle to account for factors that are difficult to quantify, such as the subtle variations in an embryo's environment or the clinical context. AI also lacks the ability to fully interpret patient history, which human embryologists consider when making decisions. Furthermore, the technology is still evolving, and it may not always provide definitive answers or predict outcomes with complete reliability.
AI tools can assist in pre-screening embryos by analyzing factors like morphology and development patterns, potentially identifying which embryos are more likely to be genetically normal. This can help limit embryos for biopsy, reducing the number of embryos that need to undergo genetic testing (PGT), which in turn could lower costs for patients. However, while AI can aid in optimizing the embryo selection process, it does not replace genetic testing itself. The role of AI is to complement PGT, not to directly determine which embryos will be genetically normal.
Patients benefit from the integration of AI in embryo grading processes through more consistent, objective, and detailed reporting. AI systems can provide comprehensive insights into the quality and development of embryos, helping patients better understand their options. This can lead to more informed decision-making and potentially reduce the emotional stress associated with IVF treatment. Additionally, by optimizing embryo selection, AI may increase the chances of successful outcomes and reduce the number of cycles needed, offering patients a more efficient and personalized approach to treatment.
AI tools offer more consistent and objective embryo grading, potentially helping in selecting higher-quality embryos. Additionally, they provide excellent and detailed reporting, enhancing the overall patient experience. However, while AI can optimize the selection process, its direct impact on improving pregnancy rate is still under study. The decision to use AI tools should depend on your financial capability. If you can afford it, AI may be a worthwhile investment for enhancing the patient experience, but it should not be relied upon as a guaranteed way to improve IVF success. Consider it as an added tool to augment decisions rather than tool that decide for you.
We understand that most standard IVF clinics provide embryo images with the embryo transfer report. For clinics that don’t include them by default, you can always request these images, as they are typically captured for internal documentation and can be shared upon request.
At our clinic, we do not include embryo images in our standard embryology report to avoid unnecessary use of paper. Additionally, most patients may not fully understand the meaning of the images or the grading system. Since embryology reports are given immediately after the embryo transfer, sharing images of embryos—whose outcome will only be known after two weeks—might feel a bit premature.
Lorem ipsum dolor sit amet, consectetur adipiscing elit. Ut elit tellus, luctus nec ullamcorper mattis, pulvinar dapibus leo.
Talk to our Expert Embryologist
Ms. Doel Bose Pande, Central India's first ESHRE Certified Senior Clinical Embryologist.
Book Free Appointment
Book a free detailed embryology consultation with our senior embryologist to understand your previous Embryology Reports and what can be done in future IVF Cycles for success
