
Infertility is a profoundly challenging journey that can inflict emotional and mental distress upon couples. Fortunately, technological advancements and medical care have led to a variety of solutions for infertility. With the best treatment options available at the IVF center in Indore, patients need not travel outside the city for treatment.
What is infertility
Causes of Infertility in Males

What are the main causes of infertility in male partner? Let’s look at the main factors of male infertility.
- Low sperm count: There are various factors that can contribute to low sperm count. These include hormonal imbalances, testicular issues, genetic factors, varicocele (enlarged veins within the scrotum), certain medical conditions like diabetes and infections, exposure to environmental toxins, excessive stress, and lifestyle factors such as smoking, alcohol consumption, drug use, and obesity.
- Abnormality in sperm function or production: Abnormalities in sperm function or production can significantly impact male fertility. These abnormalities encompass a range of issues like abnormal sperm motility or morphology that affect the sperm’s ability to fertilize an egg and support successful conception.
- Obstructions or blockages:Obstructions or blockages within the male reproductive system can hamper fertility. These blockages impede the normal flow of sperm, leading to issues with conception. Blockages can occur in crucial pathways like the epididymis, where sperm mature and are stored, or the vas deferens, responsible for transporting mature sperm.
Causes include infections, congenital conditions, scarring from injuries or surgeries, and issues like retrograde ejaculation, where semen enters the bladder instead of being ejaculated. These blockages can be diagnosed through exams and tests like ultrasounds, and treatments range from surgical correction to assisted reproductive methods like IVF with ICSI. Consulting a infertility specialist for proper evaluation is recommended for tailored guidance. - Erectile Dysfunction: Certainly! Erectile dysfunction (ED) refers to the persistent inability to achieve or maintain an erection sufficient for satisfactory sexual activity. It can stem from various factors, including physical, psychological, and lifestyle-related elements. Physical causes encompass conditions such as diabetes, cardiovascular issues, hormonal imbalances, and neurological disorders. Psychological factors like stress, anxiety, depression, and relationship problems can contribute to ED.
Lifestyle choices like smoking, excessive alcohol consumption, and sedentary habits also play a role. Effective treatments for ED range from lifestyle adjustments and counseling to medications, vacuum devices, and implants. A comprehensive assessment by a healthcare professional can help identify the underlying cause and guide towards suitable interventions, thus improving overall sexual health and well-being. - Varicocele: Varicocele refers to the enlargement of veins within the scrotum, causing them to become dilated and potentially impacting male fertility. While the exact cause is not always clear, it’s believed that faulty valves in the veins contribute to blood pooling, leading to the enlargement. This condition can raise the temperature within the testes, potentially affecting sperm production and quality. Varicoceles are often painless but can cause discomfort.
They can be diagnosed through physical exams and imaging tests. Treatment options include observation, lifestyle changes, or surgical correction to improve fertility, relieve discomfort, or prevent potential complications. Consulting a urologist or fertility specialist is advisable for accurate diagnosis and personalized guidance. - Hormonal imbalance: Hormonal imbalance refers to disruptions in hormone levels that can affect male reproductive functions and overall well-being. Testosterone, a key hormone, impacts various aspects of health. Imbalances may arise due to age, medical conditions, obesity, stress, or medications, leading to symptoms like altered libido, fatigue, mood changes, and sexual issues.
Treatments involve lifestyle changes and hormone replacement therapy under medical supervision. Consulting a healthcare professional is essential for accurate diagnosis and effective management. - Genetic disorders: Genetic disorders can play a significant role in male infertility. Conditions such as Klinefelter syndrome, Y chromosome deletions, and chromosomal translocations can impact sperm production and function.
These disorders are often inherited and can lead to reduced sperm count, abnormal sperm morphology, and impaired sperm motility. Genetic testing and counseling are crucial for identifying these conditions early and providing insights into potential reproductive challenges. - Infections: Infections can play a significant role in male infertility. Infections of the reproductive organs, such as epididymitis and sexually transmitted infections, can lead to inflammation and scarring that obstruct the flow of sperm. These conditions can impact sperm production, motility, and overall quality.
Infections can also affect the health of the sperm themselves, leading to DNA damage and reduced fertilization potential. Early diagnosis, proper treatment of infections, and maintaining sexual health are essential steps in preventing potential fertility issues caused by infections. - Obstruction: Obstructions in the male reproductive system can significantly contribute to infertility. Blockages in pathways like the epididymis or vas deferens can prevent the proper transport of sperm for ejaculation. These blockages can result from infections, congenital conditions, scarring from injuries or surgeries, or issues like retrograde ejaculation.
Obstructions can hinder sperm from reaching their intended destination, affecting the chances of successful conception. Diagnosis through exams and tests can guide appropriate treatment, which can range from surgical correction to assisted reproductive methods such as IVF with ICSI. - Lifestyle factors: Lifestyle factors play a crucial role in male infertility. Choices like smoking, excessive alcohol consumption, drug use and obesity can adversely impact sperm quality and production. Sedentary lifestyles and poor dietary choices can also contribute to obesity and related health issues that influence reproductive health.
Making informed choices and maintaining a healthy lifestyle can significantly enhance male reproductive health and increase the chances of successful conception.
Causes of Infertility in females

These are the causes of female infertility in females. Let’s look at some of the factors:
- Ovulation Disorders: Ovulation disorders are a common cause of female infertility. Irregular or absent ovulation can result from hormonal imbalances, conditions like polycystic ovary syndrome (PCOS), thyroid disorders, and excessive exercise. These disruptions prevent the release of mature eggs necessary for fertilization. Addressing ovulation disorders often involves hormonal treatments, lifestyle adjustments, and medical guidance to enhance fertility prospects.
- Blockages in Fallopian Tubes: Blockages in fallopian tubes are a notable cause of female infertility. These blockages can stem from infections, pelvic inflammatory disease, endometriosis, or scar tissue from surgeries. Blocked tubes hinder the movement of eggs and sperm, preventing successful fertilization and implantation.
Diagnosis through imaging tests helps identify the issue and treatments may involve surgical correction or assisted reproductive techniques like IVF to bypass the blockage and enhance the chances of conception. - Endometriosis: Endometriosis is a significant contributor to female infertility. This condition occurs when tissue similar to the uterine lining grows outside the uterus, often leading to pain and inflammation. Endometrial implants can affect the fallopian tubes, ovaries, and pelvic structures, interfering with egg release, sperm movement, and embryo implantation. Scar tissue and adhesions can further complicate fertility. Addressing endometriosis-related infertility might involve medications, laparoscopic surgery, or assisted reproductive techniques such as IVF, tailored to each individual’s situation.
- PCOS ( Polycystic Ovary Syndrome): Polycystic Ovary Syndrome (PCOS) is a common cause of female infertility. It’s characterized by hormonal imbalances that lead to irregular or absent ovulation. Multiple small cysts can form on the ovaries. Elevated levels of androgens (male hormones) can disrupt the normal ovulatory process. Women with PCOS may experience irregular menstrual cycles, increased facial hair, and weight gain. Managing PCOS often involves lifestyle changes, medications to regulate hormones, and fertility treatments tailored to restore ovulation and increase the chances of conception.
- Uterine abnormalities: Uterine abnormalities can contribute to female infertility. Conditions like uterine fibroids, polyps, or structural anomalies can impact fertility by affecting implantation, embryo development, or the ability to maintain a pregnancy. Fibroids and polyps can alter the uterine environment, while structural issues like septate or bicornuate uterus can hinder embryo implantation. Diagnosis through imaging helps identify these abnormalities. Treatment approaches vary and may involve surgical interventions to correct structural issues or remove growths.
- Age-related inefficiencies: Age-related factors play a significant role in female infertility. As women age, the quantity and quality of their eggs decline, leading to reduced fertility. This decline becomes more pronounced after the age of 35. Advanced maternal age increases the risk of chromosomal abnormalities in eggs, which can result in miscarriages or birth defects. Age-related inefficiencies in egg production, hormonal changes, and an increased risk of medical conditions like endometriosis or fibroids can all impact fertility.
- PID (Pelvic Inflammatory Disease):Pelvic Inflammatory Disease (PID) can contribute to female infertility. PID is often caused by untreated sexually transmitted infections, which lead to inflammation and scarring of the reproductive organs, including the fallopian tubes. This scarring can block the fallopian tubes, preventing eggs from meeting sperm and hindering fertilization.
Additionally, the inflammatory environment created by PID can impair egg quality, embryo implantation, and overall reproductive function. Early detection, prompt treatment of infections, and proper medical care are essential to prevent the long-term reproductive consequences of PID and its impact on fertility. - Thyroid disorders : Thyroid disorders can significantly impact female fertility. Both an underactive thyroid (hypothyroidism) and an overactive thyroid (hyperthyroidism) can disrupt hormonal balance, affecting ovulation and menstrual regularity. Thyroid hormones play a crucial role in reproductive health, and imbalances can lead to irregular cycles, difficulty conceiving, and an increased risk of miscarriages.
Managing thyroid disorders through medication and regular monitoring is essential to restore hormonal equilibrium and improve fertility prospects. Consulting a healthcare professional for diagnosis and appropriate treatment is vital for women facing thyroid disorder and infertility.
- POI( Premature Ovarian Insufficiency): Premature Ovarian Insufficiency (POI), also known as premature menopause, is a significant cause of female infertility. It involves the ovaries ceasing normal function before the age of 40, resulting in reduced egg quantity and quality. This condition can lead to irregular or absent menstrual cycles, hormonal imbalances, and difficulty conceiving.
While the exact cause of POI is often not clear, factors such as genetics, autoimmune conditions, and certain medical treatments can contribute. Managing POI typically involves hormone replacement therapy to address hormonal imbalances and support reproductive health. For women facing POI, assisted reproductive techniques like egg donation or adoption may be considered to achieve pregnancy. - Unexplained infertility: Unexplained infertility is a frustrating and perplexing cause of female infertility. In some cases, despite thorough medical evaluation, no clear underlying reason for infertility can be identified. Hormonal imbalances, subtle structural issues, immune factors, or other complex interactions could contribute. While the cause may remain elusive, fertility treatments like assisted reproductive techniques, such as intrauterine insemination (IUI) or in vitro fertilization (IVF), can still offer a chance of successful conception for couples facing unexplained infertility.
Infertility treatment options for Women

Let’s look at all the treatment options for Women that can cure their infertility:
Ovarian stimulation:
This treatment goes with the administration of medications for ovulation stimulation. This treatment is used for women with absent or irregular ovulation.
Common Medicines for Ovulatory problems are:
Clomiphene citrate (Clomid®), Human menopausal gonadotropin or hMG (Repronex®; Pergonal®), Follicle-stimulating hormone or FSH (Gonal-F®; Follistim®), Gonadotropin-releasing hormone (Gn-RH), Gonadotropin-releasing hormone (Gn-RH), Bromocriptine (Parlodel®).
Ovarian Stimulation is suggested when it is perceived that there are issues with ovulation.
How is Ovarian Stimulation done?

Different levels of Stimulation can be used for ovulation disorders:
- The drug clomiphene citrate (Clomid or Serophene) is taken for 5 days during the pre ovulatory phase.
- Clomiphene can be taken with intrauterine insemination to increase the medication’s effectiveness by bringing the sperm and egg closer together.
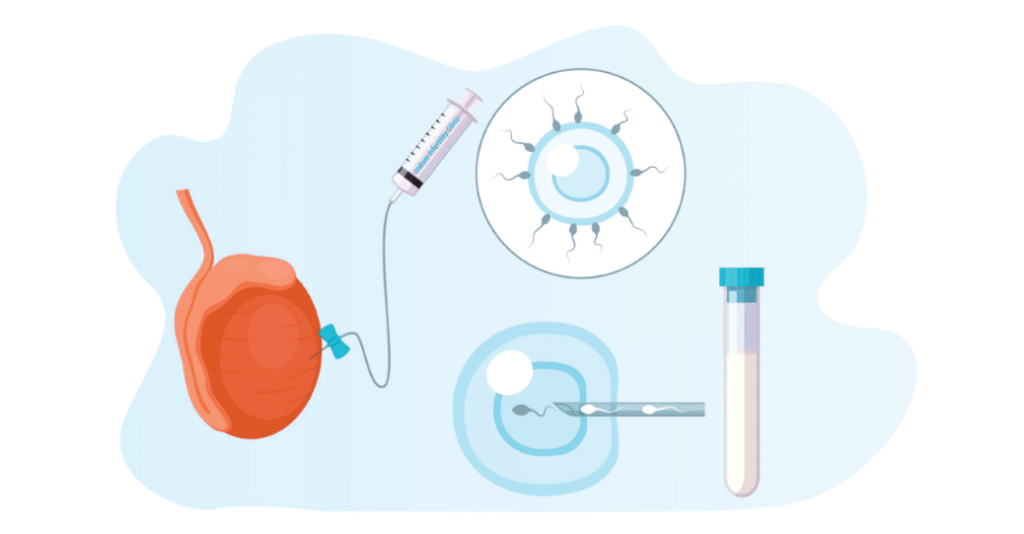
IUI or Intrauterine Insemination:
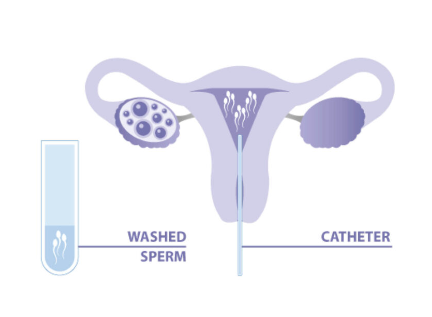
This technique involves the direct placement of concentrated and washed sperm into the uterus just before ovulation. This process can enhance the likelihood of fertilization. It is employed for women with unexplained infertility or mild male factor infertility.
This treatment is recommended for individuals with unexplained fertility, endometriosis-related infertility, subfertility and cases where the male partner has infections like HIV, hepatitis, or cervical factor infertility. It is also suggested for couples who have infrequent cohabitation or who live apart, those with semen allergies and those considering donor sperm.
How is IUI done?
UI, or intrauterine insemination, is a fertility treatment where sperm is placed directly into a woman’s uterus to enhance the chances of fertilization. It’s a common procedure at our clinic, one of the best IVF centre in Indore, led by a renowned IVF doctor. This method can be especially effective for certain fertility issues. Remember, personalized guidance from experts matters most.
After a brief rest, women can get back to their regular routines. The cost of IUI treatment in Indore is reasonable and tied to this meticulously executed process. The IUI procedure necessitates meticulous planning and precise steps to ensure favorable outcomes:
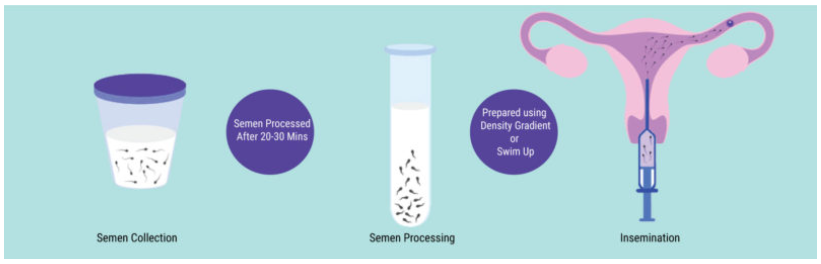
- Monitoring for ovulation: Ovulation-inducing drugs can be taken on a doctor’s prescription. Using an ultrasound the follicles are monitored
- Determining the best timing: The IUI is timed 24 hrs to 36 hrs after administration of hCG injection.
- Preparation of Semen Sample: The c is prepared by swim-up or double density gradient method.
For the best results make sure the following criteria are met:
- Patent/Open Fallopian Tubes
- The thickness of Endometrium > 7mm
- Size of Follicle > 18 mm
- Total count of Motile Sperm > 10 Million
IVF or In Vitro Fertilization:
IVF, or In vitro fertilization, is a fertility treatment where eggs and sperm are combined outside the body in a lab dish. After fertilization, the resulting embryos are then carefully implanted into the uterus. For top-notch IVF results, consider visiting the best IVF clinic in Indore.
What is Test Tube Baby Procedure? Is it the same as IVF?
Yes, the term Test Tube baby procedure and IVF is the same thing and can be used interchangeably.
How is IVF done?
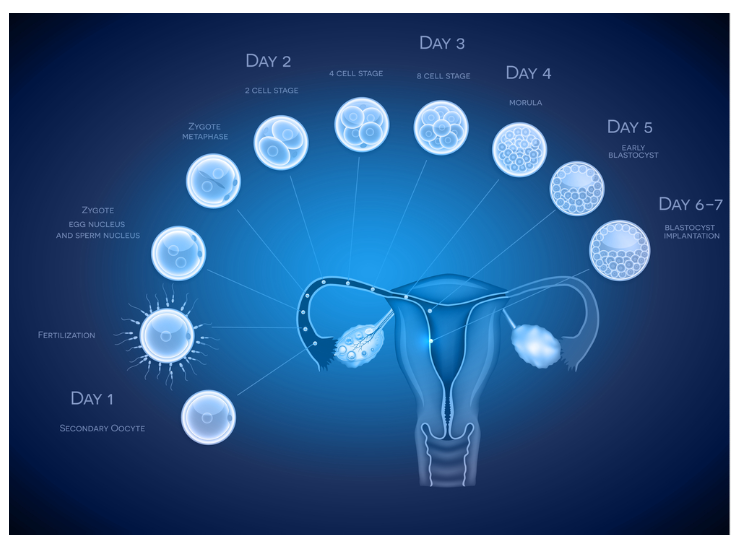
In vitro fertilization (IVF) has revolutionized fertility treatments. It offers hope to couples facing challenges in conceiving naturally.
IVF involves a series of carefully orchestrated steps that culminate in the creation of life. Below are the key stages of the IVF process:
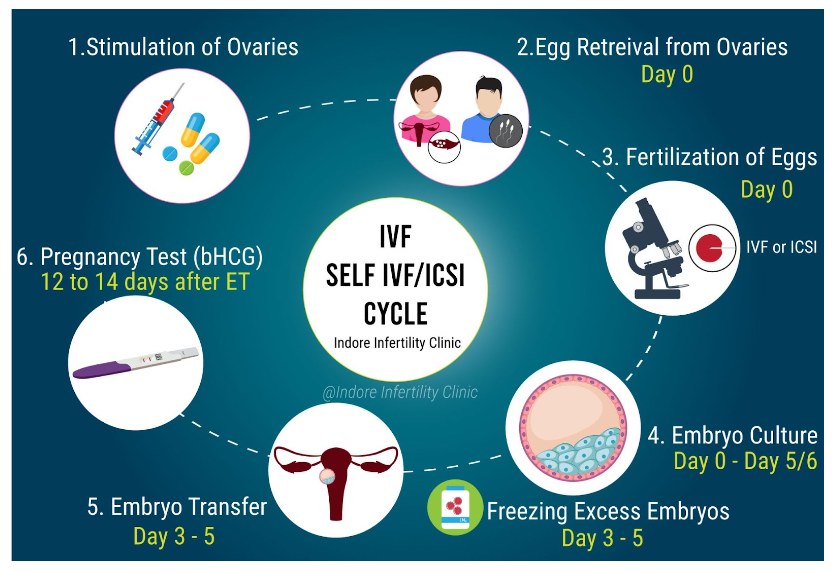
- Ovarian Stimulation: Fertility medications are administered to stimulate the ovaries, encouraging the production of multiple eggs.
- Egg Retrieval: Through a minimally invasive procedure, mature eggs are gently collected from the ovaries.
- Sperm Collection: A sperm sample is obtained from either the male partner or a donor.
- Fertilization: In a controlled laboratory environment, eggs and sperm are combined to facilitate fertilization.
- Embryo Cultivation: The resulting embryos are closely monitored and cultured for several days.
- Embryo Transfer: One or more healthy embryos are carefully selected and transferred into the uterus.
- Waiting Period: A short span of anticipation follows as the hopeful parents await news of successful implantation and pregnancy.
When considering IVF, selecting the right clinic plays a pivotal role. Discover excellence in fertility care at the best IVF clinic in Indore.
What is IVF pregnancy?
IVF pregnancy refers to a successful pregnancy achieved through the process of In vitro fertilization (IVF), where fertilization of eggs and sperm occurs outside the body in a lab dish, followed by the implantation of resulting embryos into the uterus.
Cost of IVF treatment?
The cost of IVF treatment can vary based on several factors, including the specific procedures required, medications, and lab services. In Indore, the cost of IVF treatment is influenced by the expertise and facilities offered by the chosen clinic. It’s advisable to thoroughly discuss the IVF treatment cost in Indore with the best clinic to gain a comprehensive understanding of the expenses involved and the potential outcomes.
PRP Therapy
What is PRP therapy?

Platelet-Rich Plasma (PRP) therapy is an innovative approach in the realm of regenerative reproduction. By harnessing the potent growth factors found in a patient’s own blood, PRP therapy promotes tissue repair and rejuvenation in reproductive contexts.
This technique involves drawing a small blood sample, concentrating platelets, and then strategically injecting them into the targeted reproductive area. Through this process, PRP therapy aims to stimulate natural healing mechanisms, potentially aiding in addressing fertility challenges and optimizing reproductive health due to low ovarian reserve or poor endometrium.
How can PRP therapy be used in infertility patients?
PRP therapy holds promise as a complementary approach in treating infertility. For infertility patients, PRP therapy can be utilized to potentially enhance reproductive outcomes through the following avenues:
- Ovarian Rejuvenation: PRP injections into the ovaries might stimulate follicular growth and improve egg quality, potentially increasing the chances of successful fertilization.
- Endometrial Health: PRP therapy could be employed to improve the thickness and receptivity of the endometrial lining, creating a more conducive environment for embryo implantation.
- Supporting IVF: PRP injections during IVF procedures might enhance embryo implantation by improving the uterine environment.
- Male Infertility: PRP therapy might aid in treating certain cases of male infertility by promoting the growth of healthy sperm cells.
However, it’s important to note that while PRP therapy shows promise, its efficacy and safety in infertility treatment are still being studied. Consulting with reproductive specialists at the best IVF clinic in Indore is crucial for informed decisions tailored to individual patient needs.
How is PRP Therapy done?
PRP therapy involves several steps to harness the regenerative potential of platelet-rich plasma:
- Blood Collection: A small amount of the patient’s blood is drawn, typically from the arm.
- Processing: The blood sample is placed in a centrifuge to separate its components. This process isolates the platelet-rich plasma, which is rich in growth factors.
- Platelet Activation: The isolated PRP is activated, releasing growth factors that play a crucial role in tissue repair and regeneration.
- Injection: The activated PRP is carefully injected into the targeted area using sterile techniques. In reproductive contexts, this could include the ovaries, uterine lining, or other relevant areas.
- Healing Response: The growth factors in the PRP trigger a natural healing response, promoting cellular repair, improved blood flow, and tissue rejuvenation.
- Monitoring: Regular follow-up appointments help monitor progress and determine the need for additional treatments.
It’s important to note that the specifics of PRP therapy can vary based on the patient’s condition and the medical professional’s expertise. For personalized guidance on PRP therapy for infertility, consulting with experts at the best IVF clinic in Indore is recommended.
Oocyte Freezing / Egg Freezing or Social Freezing
Oocyte freezing, commonly known as egg freezing or social freezing, is a fertility preservation technique that allows individuals to preserve their eggs for future use. This method involves stimulating the ovaries to produce multiple eggs, which are then carefully extracted, frozen, and stored.
Oocyte freezing provides an option for women to delay childbearing while retaining the potential to use their own healthy eggs later in life. This can be particularly beneficial for those focusing on career or medical reasons. Consulting experts at the best IVF clinic in Indore can provide valuable insights into this fertility preservation approach.
How Egg freezing can be used for infertile patients?
Egg freezing serves as a valuable option for infertile patients seeking to overcome fertility challenges:
- History of Menopause: Egg freezing provides an opportunity for women with a history of menopause or premature ovarian insufficiency to preserve viable eggs for future use.
- Cancer Treatment: Infertile patients facing cancer treatments like chemotherapy or radiotherapy, which can impact fertility, can safeguard their reproductive potential through egg freezing.
- Career Goals: Individuals prioritizing career aspirations can opt for egg freezing, allowing them to delay childbearing while securing the option to use their healthy eggs later.
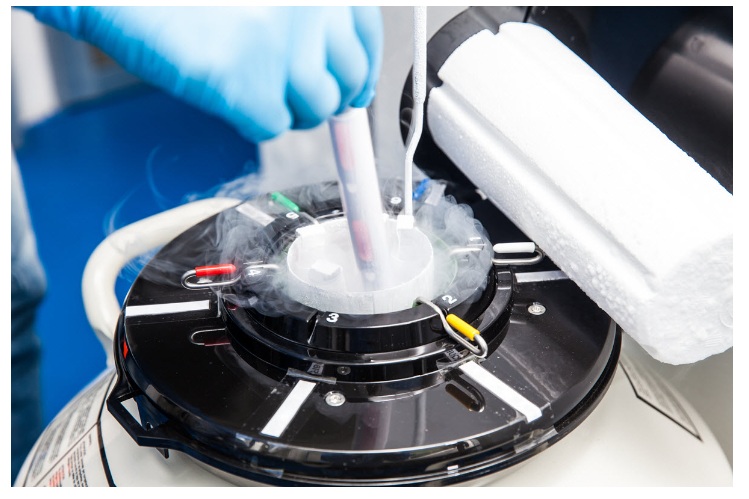
How is egg freezing done?
Egg freezing, also known as oocyte cryopreservation, involves a carefully orchestrated process to preserve a woman’s fertility. The procedure typically follows these steps:
- Ovarian Stimulation: Fertility medications are administered to stimulate the ovaries, encouraging the production of multiple eggs.
- Egg Retrieval: Once the eggs are mature, a minimally invasive procedure retrieves them from the ovaries using a thin needle guided by ultrasound.
- Cryopreservation: The collected eggs are then rapidly frozen using a method called vitrification, which helps prevent ice crystal formation that can damage the delicate egg structure.
- Storage: The frozen eggs are stored in specialized cryogenic tanks at extremely low temperatures until they are needed.
Egg freezing offers women the opportunity to preserve their fertility for future family planning.
Is Egg freezing Safe
Egg freezing, a well-established technique, is generally considered safe and has been used successfully for years. Advanced freezing methods like vitrification have significantly improved egg survival rates during the thawing process. While no medical procedure is entirely risk-free, complications from egg freezing are rare. Potential risks include a small chance of infection, discomfort from the retrieval procedure, or hormonal side effects.
Consulting with fertility specialists at the best IVF clinic in Indore can provide a comprehensive understanding of the safety measures in place and personalized insights based on individual health factors.
What is the cost of Freezing Eggs or Oocyte /Egg Freezing?
The cost of freezing eggs, also known as oocyte or egg freezing, can vary based on factors such as location, clinic expertise, and the specific services included. It’s important to note that the cost of egg freezing is often comparable to that of an IVF cycle, encompassing various stages like ovarian stimulation, egg retrieval, and lab procedures.
Additionally, there are charges associated with the cryopreservation of eggs for years, which typically involves ongoing storage fees. Consulting the best fertility specialists can offer transparency regarding the costs involved and help individuals make informed decisions aligned with their reproductive goals.
What is Blastocyst Culture
Blastocyst culture is a pivotal technique in assisted reproductive technology that involves cultivating embryos in a laboratory setting for an extended period. This process allows embryos to develop more comprehensively and reach the blastocyst stage, which typically occurs around day five or six days post-fertilization.
During blastocyst culture, embryologists closely monitor embryo growth, assessing their quality and selecting the healthiest ones for transfer into the uterus. This approach increases the likelihood of successful implantation and pregnancy.
When is the Blastocyst Culture done?
Blastocyst culture is strategically employed in specific scenarios:
- Previous IVF Failure: When standard IVF cycles have not resulted in successful pregnancies, blastocyst culture offers a more advanced approach to selecting the healthiest embryos, potentially increasing the chances of implantation.
- Elective Single Embryo Transfer (eSET): Blastocyst culture aids in identifying the strongest embryo for transfer, making eSET a viable option to reduce the risk of multiple pregnancies while maintaining high success rates.
- Advanced Maternal Age: Older patients might benefit from blastocyst culture as it allows embryologist to choose the most viable embryo, compensating for the potential decrease in egg quality associated with advanced maternal age.
How is Blastocyst Culture Done?
Blastocyst culture involves a methodical approach to enhance embryo development:
- Fertilization: After fertilization, embryos are cultured in a controlled environment.
- Extended Cultivation: Embryos are cultured for about 5-6 days, allowing them to reach the blastocyst stage.
- Selection: Embryologists assess embryo development and select the healthiest blastocysts based on morphology and other criteria.
- Embryo Transfer: Selected blastocysts are transferred into the uterus during a carefully timed procedure, aligning with the embryo’s natural implantation window.
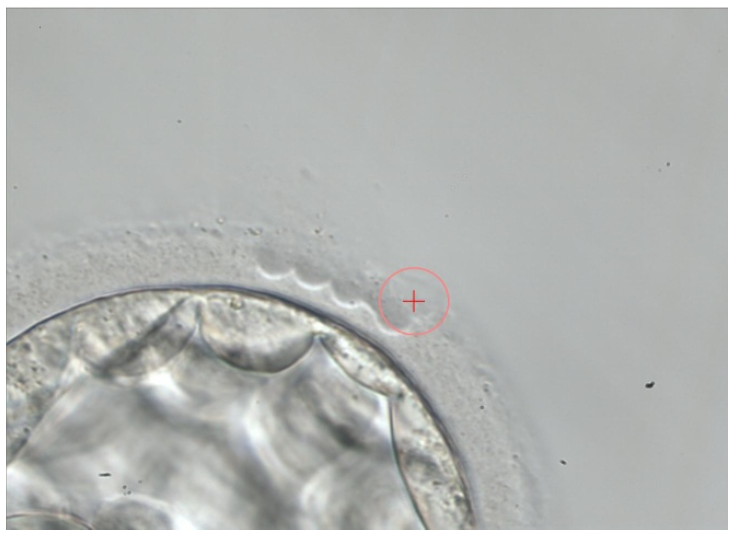
What is Laser Assisted Hatching ?
Laser-assisted hatching is a specialized reproductive technique aimed at enhancing the chances of embryo implantation during in vitro fertilization (IVF). This method involves using a precise laser to create a small opening or thinning in the outer shell of an embryo, known as the zona pellucida. By facilitating the embryo’s exit from this protective shell, laser-assisted hatching can potentially improve the embryo’s ability to attach to the uterine lining and initiate a successful pregnancy.
This technique is particularly considered for cases where the zona pellucida is abnormally thick or when previous IVF attempts have shown challenges in implantation. For comprehensive insights into whether laser-assisted hatching is appropriate, consulting experts at the best IVF doctor in Indore is advised.
When is Laser Assisted Hatching Done?
Laser-assisted hatching is considered in specific scenarios:
- Thick Zona Pellucida: When the embryo’s outer shell (zona pellucida) is abnormally thick, laser-assisted hatching can aid in creating an opening for successful embryo implantation.
- Advanced Maternal Age: Older patients may benefit from this technique, as the zona pellucida can sometimes become harder with age, potentially hindering implantation.
- Previous IVF Failure: If previous IVF cycles have not resulted in pregnancy, laser-assisted hatching can be explored to potentially improve the chances of implantation.
- Frozen Embryo Transfer: Laser-assisted hatching might be considered when transferring frozen-thawed embryos to enhance their implantation potential.
How is Laser Assisted Hatching done ?
Laser-assisted hatching involves these key steps:
- Embryo Selection: Embryos are carefully selected based on criteria like quality and developmental stage.
- Precise Laser Application: A focused laser beam is used to create a controlled opening or thinning in the zona pellucida, the embryo’s outer shell.
- Minimized Thermal Impact: The laser’s precision ensures minimal heat transfer, preventing potential damage to the embryo.
- Embryo Transfer: Following laser-assisted hatching, the selected embryo is transferred into the uterus during an IVF cycle.
What is IVF with Donor Egg Program ?
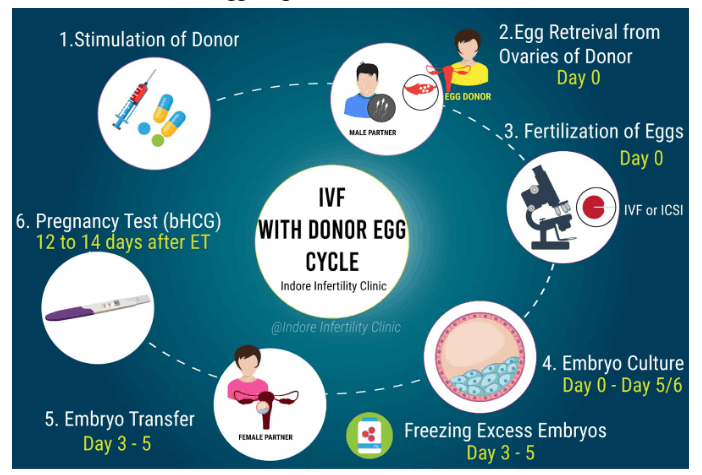
IVF with Donor Egg Program is a fertility treatment option that involves using donor eggs from a carefully screened and healthy donor to create embryos. This approach is typically considered when a woman’s own eggs are not viable due to advanced age, poor egg quality, or medical conditions. During the procedure, the donor egg are fertilized with sperm from either the male partner or a sperm donor, and the resulting embryos are then transferred into the recipient’s uterus.
For those seeking this solution, the best IVF center in Indore can provide expert guidance and support throughout the IVF with Donor Egg Program, ensuring a comprehensive approach to fertility treatment.
When is a Donor egg recommended?
Donor egg recommendation typically occurs in the following scenarios:
- Advanced Maternal Age: Women in their late 30s or older might consider donor eggs due to decreased egg quality and diminished ovarian reserve.
- Poor Egg Quality: Individuals with eggs of lower quality, affecting fertilization and embryo development, may benefit from donor eggs.
- Genetic Conditions: Couples with a history of genetic disorders might opt for donor eggs to mitigate the risk of passing on hereditary conditions.
- Unsuccessful IVF Attempts: When multiple IVF cycles with a woman’s own eggs have resulted in unsuccessful pregnancies, donor egg might be explored as an alternative.
- Premature Ovarian Insufficiency: Women experiencing premature menopause or diminished ovarian function may find donor eggs a viable solution.
How is the Process of egg donation done?
The egg donation process involves several key steps:
- Donor Selection: Egg donors are carefully selected based on their medical history, genetics, and overall health. They undergo thorough screening, including physical and psychological assessments.
- Cycle Synchronization: The donor’s menstrual cycle is synchronized with the recipient’s cycle using medications, ensuring optimal timing for embryo transfer.
- Ovarian Stimulation: The donor receives fertility medications to stimulate the ovaries for producing multiple eggs in a single cycle.
- Egg Retrieval: Once the eggs are mature, a minimally invasive procedure retrieves them from the donor’s ovaries.
- Fertilization: The donor eggs are fertilized with sperm from the recipient’s partner or a sperm donor in the laboratory.
- Embryo Transfer: The resulting embryos are cultured and monitored for quality before being transferred into the recipient’s uterus.
What is Surrogacy ?

Surrogacy is a collaborative reproductive arrangement where a woman (the surrogate) carries and gives birth to a child on behalf of another person or couple (the intended parents). It’s a viable option when traditional pregnancy is not possible or advised. There are two main types:
- Gestational Surrogacy:In gestational surrogacy, the surrogate carries an embryo created using the egg of the intended mother or an egg donor, and sperm from the intended father or a sperm donor.
The surrogate has no genetic relation to the child she carries.
- Altruistic Surrogacy:Altruistic surrogacy involves a surrogate who doesn’t receive monetary compensation beyond covering medical expenses and related costs.The motivation is purely to help a couple or individual experience parenthood.
Surrogacy offers hope for those facing fertility challenges and is regulated by legal agreements to ensure the rights and responsibilities of all parties involved.
You can trust indore infertility clinic when it comes to the Surrogacy treatment in Indore.
Is Surrogacy for Me ? Things to consider
Embarking on the surrogacy journey is a significant decision with multifaceted considerations. Here are vital aspects to ponder:
Financial Considerations:
Costs: Surrogacy involves substantial financial commitments, covering medical fees, legal expenses, and compensating the surrogate.
Budget: Carefully assess your financial readiness, factoring in unexpected expenses and potential delays.
Legal Considerations:
Legal Agreements: Establishing legally binding contracts is crucial to defining rights, responsibilities, and expectations for all parties.
Parental Rights: The legal process varies by jurisdiction, affecting how parental rights are established for intended parents.
Emotional Preparedness:
Expectations: Surrogacy journeys can be emotionally intense. Clarify your expectations, openly communicating with the surrogate and your support network.
Flexibility: Surrogacy timelines can shift due to medical, legal, or personal reasons. Emotional flexibility is vital.
Relationship Dynamics:
Intimacy: Establishing a rapport with the surrogate is essential for a smooth journey. Open and honest communication can help build trust.
Support System: Ensure you have a strong network, including family, friends, or therapists, to lean on throughout the process.
Medical Considerations:
Health Risks: Surrogates undergo medical procedures and potential health risks. Prioritize the surrogate’s well-being throughout.
Medical Expertise: Choosing a reputable fertility clinic and experienced medical professionals is vital for successful outcomes.
Long-Term Planning:
Child’s Perspective: Consider how you’ll communicate your child’s surrogacy origin. Openness and honesty can help them navigate their identity.
Cultural and Ethical Values:
Cultural Sensitivity: Discuss and align cultural values with the surrogate, ensuring a respectful and harmonious journey.
Ethical Reflection: Reflect on the ethical dimensions of surrogacy, including considerations around exploitation and consent.
Legal and Ethical Obligations:
Legal Compliance: Adhere to legal regulations, ensuring your surrogacy arrangement respects the law.
Ethical Conduct: Treat the surrogate with respect, acknowledging her role in this transformative process.
Realistic Expectations:
Outcome: Understand that despite careful planning, surrogacy outcomes may vary. Be prepared for different scenarios.
Deciding if surrogacy is right for you involves comprehensive exploration, open communication, and thoughtful planning. Consulting with experienced professionals, including legal experts and fertility specialists, can provide you with tailored guidance aligned with your unique circumstances.
Surrogacy Law in India
Under Indian Law, only Altruistic Surrogacy is legal.
Please visit our blog on Surrogacy Act to know more : Surrogacy Laws In India
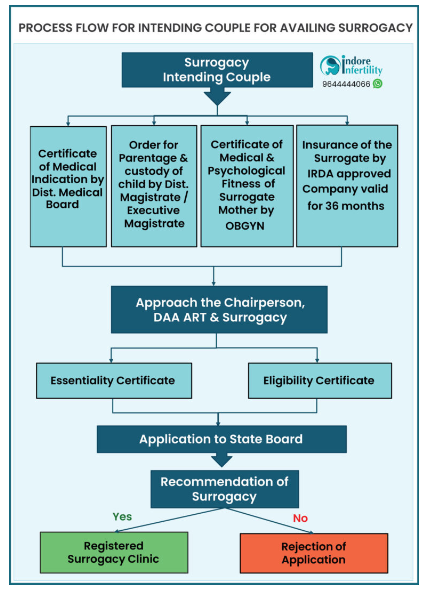
Cost of Surrogacy in Indore
4 major costs are involved in Surrogacy treatment cost in Indore- Registration of Surrogate
- IVF procedure cost
- Antenatal care and cost of the delivery
- Insurance coverage for surrogate
- Legal and documentation fees
Infertility treatment for men

Let’s look at all the treatment options for males, that can cure their infertility:
Intracytoplasmic Sperm Injection ( ICSI )
Intracytoplasmic Sperm Injection (ICSI) is an advanced fertility technique employed within in vitro fertilization (IVF). It involves the direct injection of a single sperm into an egg’s cytoplasm using a delicate microneedle. ICSI is particularly beneficial in cases of male infertility, where sperm quality or quantity is compromised. This method ensures that fertilization occurs even if the sperm’s ability to penetrate the egg naturally is hindered. ICSI has revolutionized assisted reproductive technology, offering hope to couples facing complex fertility challenges.

When is this procedure of ICSI recommended?
ICSI is recommended in various scenarios:
- Male Factor Infertility: When sperm quality, count, or motility is compromised, ICSI ensures successful fertilization by directly injecting a single healthy sperm into the egg.
- Previous Fertilization Failures: Couples who have experienced multiple failed IVF cycles due to poor fertilization might benefit from ICSI to overcome fertilization challenges.
- Sperm Retrieval Difficulties: In cases where sperm cannot be obtained through ejaculation due to medical conditions, ICSI can utilize sperm extracted directly from the testicles or epididymis.
- Frozen Sperm: ICSI can be applied when using frozen-thawed sperm, which might have reduced motility, to optimize the chances of fertilization.
- Genetic Concerns: Couples with a history of genetic abnormalities or chromosomal issues might opt for ICSI to minimize the risk of passing these conditions to their offspring.
Consulting fertility specialists at the best IVF clinic in Indore can provide individualized recommendations on when ICSI is the most suitable approach, tailored to specific medical histories and needs.
How is the ICSI procedure performed?
The ICSI procedure involves the following steps:
- Egg Retrieval: Eggs are retrieved from the ovaries using a minimally invasive procedure.
- Sperm Collection: A sperm sample is obtained from the male partner or a sperm donor.
- Microinjection: Using a specialized microneedle, a single sperm is carefully injected directly into the cytoplasm of an individual egg.
- Incubation: The injected eggs are cultured in a controlled laboratory environment to monitor fertilization.
- Embryo Transfer: Once fertilization occurs and embryos develop, a healthy embryo is transferred into the uterus during an IVF cycle.
What is Sperm Freezing ?

Sperm freezing, also known as sperm cryopreservation, is a fertility preservation technique that involves carefully collecting, processing, and freezing sperm for future use. This method is particularly
valuable for men facing medical treatments that might impact their fertility, such as chemotherapy or surgery. By freezing and storing sperm, individuals can retain the option to use their healthy sperm for assisted reproductive procedures, like in vitro fertilization (IVF), at a later time. Sperm freezing ensures the preservation of fertility potential, offering hope to those navigating medical challenges.
Why is Sperm freezing done?
Sperm freezing is performed for various reasons:
- Medical Treatments: Men undergoing medical procedures like chemotherapy or radiation, which might affect sperm production, can preserve their fertility through sperm freezing.
- Fertility Preservation: Individuals planning for vasectomy or other procedures can freeze sperm to ensure future fertility options.
- Occupational Risks: Men in hazardous work environments or military service might freeze sperm to mitigate potential reproductive risks.
- Infertility Treatment: Men with variable sperm parameters can freeze sperm as a precautionary measure before infertility treatments like IVF.
- Age and Lifestyle: Older men or those with lifestyle factors affecting sperm quality might opt for sperm freezing to secure fertility potential.
What is TESA / PESA – SPERM EXTRACTION ?
TESA (Testicular Sperm Aspiration) and PESA (Percutaneous Epididymal Sperm Aspiration) are specialized techniques used for azoospermia treatment in Indore. These methods are particularly beneficial for men facing obstructive azoospermia or non-obstructive azoospermia, conditions where sperm is absent in the ejaculate.
TESA involves directly aspirating sperm from the testicle using a fine needle, while PESA involves extracting sperm from the epididymis. These procedures enable men to have a chance at biological fatherhood by utilizing their sperm for assisted reproductive techniques like intracytoplasmic sperm injection (ICSI). For tailored insights into azoospermia treatment and the suitability of TESA/PESA, consulting experts at the best IVF clinic in Indore is recommended.
How is TESA/PESA performed?
TESA (Testicular Sperm Aspiration) and PESA (Percutaneous Epididymal Sperm Aspiration) involve the following steps:
TESA (Testicular Sperm Aspiration):
- Anesthesia: Local anesthesia is administered to numb the area.
- Needle Aspiration: A fine needle is inserted into the testicle to aspirate small amounts of testicular tissue containing sperm.
- Sperm Retrieval: The aspirated tissue is processed in the laboratory to isolate viable sperm.
- Sperm Selection: High-quality sperm are selected for use in assisted reproductive techniques like ICSI.
PESA (Percutaneous Epididymal Sperm Aspiration):
- Anesthesia: Local anesthesia is applied to the area where sperm will be retrieved.
- Needle Aspiration: A thin needle is used to puncture the epididymis, a coiled tube near the testicle, to extract sperm.
- Sperm Collection: The retrieved fluid containing sperm is processed in the laboratory to separate and prepare the sperm for use in ICSI.
Both TESA /PESA sperm extraction offer solutions for men with azoospermia, enabling them to have a chance at biological fatherhood through advanced fertility treatments. Seeking expert guidance from the best IVF clinic in Indore is crucial to ensuring the proper execution of these procedures.
What is the cost of Sperm Freezing or What is the cost of TESA or Surgical
Sperm Retrieval / Extraction?
The cost of sperm freezing, TESA (Testicular Sperm Aspiration), and surgical sperm retrieval/extraction as part of azoospermia treatment in Indore can vary based on several factors, including the specific clinic, expertise, and services offered. Sperm freezing typically involves a fee for the collection, processing, and storage of sperm. For TESA or surgical sperm retrieval, costs encompass the procedure itself, anesthesia, medical team, and laboratory processing. To gain clarity on the azoospermia treatment costs in Indore for sperm freezing or surgical sperm retrieval, consulting fertility specialists at the best IVF clinic in the region is recommended. They can provide detailed insights into pricing structures and help you make well-informed decisions tailored to your unique situation.
What is Micro TESE – Testicular Sperm Extraction ?
Micro-TESE (Microscopic Testicular Sperm Extraction) involves the following steps:
- Precision Surgery: Unlike traditional TESE, micro-TESE employs high-powered microscopes for precise identification of areas likely to contain sperm.
- Minimized Tissue Damage: Micro-TESE extracts the smallest tissue samples needed, reducing tissue damage while maximizing the chances of finding viable sperm.
- Optimal Sperm Retrieval: The surgical procedure aims to locate viable sperm within the testicles of men with non-obstructive azoospermia.
How is it performed?
Micro-TESE (Microscopic Testicular Sperm Extraction) involves the following steps:
- Microscopic Exploration: High-powered microscopes are used to examine the testicular tissue in detail, identifying areas likely to contain viable sperm.
- Precision Extraction: The surgeon makes minimal incisions in the testicular tissue to extract the smallest samples needed to locate sperm.
- Laboratory Processing: The extracted tissue samples are carefully processed in the laboratory to identify and isolate viable sperm.
- Advanced Fertility Treatment: Viable sperm retrieved through micro-TESE can be used for specialized assisted reproductive techniques like intracytoplasmic sperm injection (ICSI).
This advanced surgical technique offers a promising option for men with non-obstructive azoospermia, providing them with the opportunity to use their sperm for fertility treatments.
What is the cost of Micro TESE or What is the cost of Surgical Sperm Retrieval
The cost of Micro-TESE (Microscopic Testicular Sperm Extraction) or surgical sperm retrieval can vary depending on factors such as the specific clinic, the expertise of the medical team, and the services included. Surgical sperm retrieval procedures often encompass expenses related to the surgery itself, anesthesia, medical staff, and laboratory processing. To gain a clear understanding of the cost of Micro-TESE or surgical sperm retrieval, it’s advisable to consult fertility specialists in indore at the best IVF clinic in Indore
conclusion
Indore IVF clinic offers a range of infertility treatment options for both males and females. Whether you’re seeking the IVF centre in Indore or the finest IVF doctor in the city, place your trust in Indore Infertility Clinic for comprehensive and effective solutions.
